A research team at the Wyss Institute for Biologically Inspired Engineering at Harvard University have used their new ‘organ-on-a-chip’ technology to develop a model of the human airway so that diseases such as COPD can be studied outside of the human body to allow researchers to gain new insights into the disease mechanisms, identify biomarkers and test new drugs.
Diseases such as COPD and asthma are inflammatory reactions in the lungs whether to smoking, inhaled particles or bacterial/viral infections. It is already known that many of the disease processes occur in the alveoli however much less is known about how inflammation starts off these reactions and why these processes react in the way that they do. For example the reason why the body recruits white blood cells and the build-up of mucus, both of which compromises the patient’s lungs or the cause and reasoning behind exacerbations.
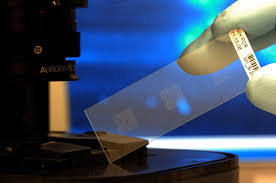
A new microfluidic model of the lung has been created of the lung’s small airways made with chips lined with cells from both normal donors and diseased patients. This model is like looking inside an actual patient and “recapitulates critical features of asthma and COPD with unprecedented fidelity and detail” explains Donald Ingber. Now with this micro-engineered human lung small airway lung inflammatory diseases over several weeks can be studied in order to gain better insight into disease mechanisms, as well as screen for new therapeutic drugs.
This device closely mimics the 3D cellular architecture of an actual human small airway and contains fully matured human small airway epithelium with different cell types and channels containing all the components that you have in your lungs including white blood cells and nutrients. The device can keep itself ‘alive’ for a few weeks before starting to deteriorate. Inflammatory situations such as asthma and COPD can be simulated by adding an asthma-inducing immune factor or by setting up the system with lung epithelial cells from a COPD patient and then researchers can observe the different ways that the airways react in different situations. In both cases, the team was not only able to observe highly disease- and cell type-specific changes but could also exacerbate them with agents simulating viral or bacterial infection.
Demand for such a device is high due to the fact that the inflammatory response is so complex and internalised that it cannot be adequately studied in humans or animals and there are no known drugs that can stop and start the inflammation processes so that you could potentially get a snap-shot of what was going on.
This new organ-on-a-chip technology has provided researchers with a window on a molecular scale to be able to observe the activities of living human tissue and allows them to break down the processes and interactions of specific cell types and immune system components so as to understand why the diseases progress in the way they do and ideas on how this could be prevented based on the interactions between the lung tissue and the immune system, whether this be by manipulating the immune system response or by developing new drugs to counteract the effects.
“This novel ability to build small airway chips with cells from individual patients with diseases like COPD positions us and others now to investigate the effects of genetic variability, specific immune cell populations, pharmaceutical candidates and even pandemic viruses in an entirely new and more personalized way; one that will hopefully increase the likelihood of success of future therapeutics,” said Ingber.
References: http://medicalxpress.com




