10 tips for winter
Cold, dry air and an increased risk of upper respiratory infections can worsen asthma symptoms during the winter. Washing your hands frequently, exercising indoors, and taking other healthy steps can help you keep a handle on asthma attacks.
- Wash your hands!
- Don’t sit by the fireplace. “The more evidence we have, the more we realize that burning wood is like burning tobacco,” explains Todd Rambasek, MD, of ENT & Allergy Health Services in Cleveland.
- Keep your mouth closed. Ideally, you want to breathe through your nose, not your mouth, when you’re out in the cold because the nose warms up the air for the lungs, Dr. Rambasek says.
- Replace filters. Your home heating system may blow dust and debris throughout your house, especially when you first start it up for the winter. It’s important to clean and replace filters before turning on your system so as not to release the debris.
- Exercise indoors. On days when it’s bitterly cold outside and the wind chill makes it feel like it’s below zero, Li recommends going to the gym instead of exercising outside. “The temperatures and the humidity in the gym are less likely to cause a problem,” she says.
- Warm up before working out. A recent study showed that people with asthma recover faster and have greater lung function after exercising when they are warmed up.
- Take steps to prevent asthma flares. Take a preventive dose of your asthma medicine before heading outside, whether to exercise, walk the dog, or run errands.
- Have an asthma action plan. No matter what the season, you should always know what to do if your asthma symptoms flare.
- Take your medications. It’s important to follow your treatment plan regardless of the time of year. Don’t let a busy work or social schedule cause you to ignore your health.
Keeping your asthma under control may take a little more effort in the cold of winter, but these strategies should get you through the season without worsened symptoms.
References: http://www.everydayhealth.com/
Natural ways to keep your oxygen levels up
Lung diseases belong to the most common disorders worldwide, with many varieties, from temporary infections to chronic diseases like chronic asthma and the progressive COPD. Patients suffering from any of these, are often prescribed strong medicines that often have many side effects. Of course these medicines also have their benefits, but for many lung disorders there are also more natural alternatives, that can help keeping your lungs in the best possible condition and ease the breathing without the burden of side effects.

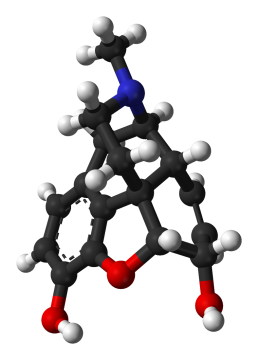
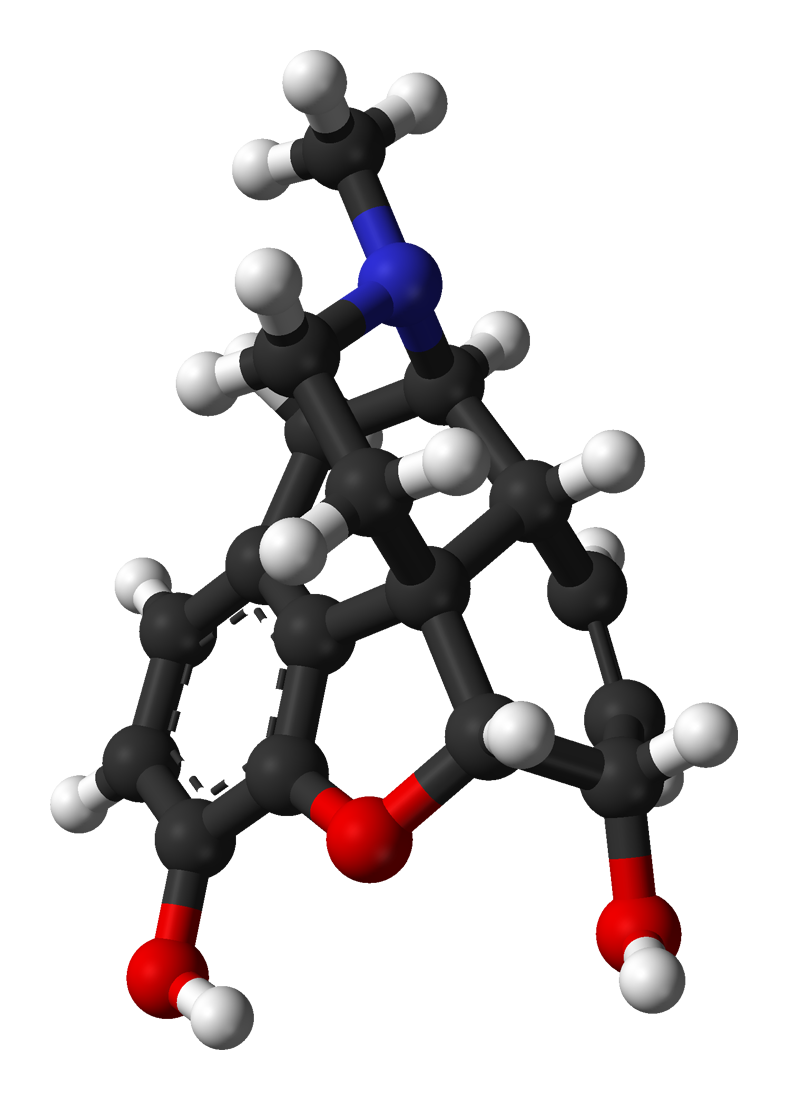
Eucalyptus against acute bronchitis
Everybody catches a cold once in a while. Actually this is a healthy phenomenon, that urges your body to a good clean up. But sometimes you just can't get rid of it and it results in a persistent dry cough. This could be an acute bronchitis; an infection of the bronchi, the large and medium sized airways in the lungs. A simple but effective remedy for this is Eucalyptus. The active ingredient in Eucalyptus is cineole, also known as eucalyptol, amongst other names. Cineole is expectorant, anti-inflammatory and dilates the bronchi by relaxing them. This was proven in a research program where patients were given pills with cineole or a placebo. The group that received the cineole pills recovered significantly faster than the placebo group. An alternative to cineole pills is eucalyptus oil; a few drops in a bowl of hot water make a wonderful steam bath, that reliefs your symptoms.
Coltsfoot to relief emphysema
Emphysema is an incurable progressive lung disease, causing shortness of breath and cough with sputum production. Coltsfoot, is traditionally used for treating obstruction of the airways. Its scientific name is Tussilago farfara, where Tussilago is derived from the latin tussis meaning cough, and ago meaning to act on. Both flowers and leaves can be used to make an infusion that relieves the coughing. A warning is in its place here, as Tussilago farfara contains tumorigenic pyrrolizidine alkaloids and can cause liver diseases in infants. A new variety called Tussilago farfara ‘Wien’ has been developed and registered, which has no detectable levels of these alkaloids and can be used safely.
Magnesium benefits asthma patients
A well performed study with 55 asthma patients, both male and female, showed that magnesium supplements are beneficial for mild to moderate asthma sufferers. From the two groups, one receiving magnesium and the other receiving a placebo, the first showed a significant improvement in their lung function and general quality of life.
Salt treatment for bronchitis
Bronchitis is a chronic disease characterised by a permanent enlargement of parts of the airways leading to the lungs. Main symptoms are a chronic cough productive of mucus and shortness of breath. There is little treatment for this disease, but lately a completely natural therapy with salt appears very promising. This so called Halotherapy, derived from the Greek ‘halos’, which means salt, has actually been used for millennia in ancient salt caves in Eastern Europe. The atmospheric salt concentrations of these caves are being reproduces in salt chambers, where walls, ceiling and floor are covered with salt. The salty air is said to be beneficial for lungs and airways and can relieve the symptoms of many lung diseases, especially those of bronchiectasis.
Lung infections can be battled with oregano oil
The essential oil of oregano is an effective remedy for both bacterial as fungal infections of the airways. It contains thymol and carvacrol, both substances of which has been scientifically proven that they inhibit the growth of bacteria and fungi. In tests on 25 different bacteria strains the essential oil was highly efficacious on all of them. The oil of Origanum syriacum, a species from the mint family native to the Middle East, is especially rich in thymol and carvacol. Supplements containing this oil can be easily obtained. If you want to use the pure essential oil, it is wise to consult a registered natural healer, who can advise you on the best suitable way and dosage. Also keep in mind that essential oils can trigger allergic reactions in some people.
Ref: Medisch dossier, Sept. 2016; Wikipedia
A healthy lifestyle also helps to keep your lungs healthy!
We all know that a healthy lifestyle can help us lose weight, get more energy and give us a better quality of life in general. But it is little known that good exercise and healthy food is especially beneficial for the well-being of your lungs also, both for people who still have healthy lungs as for people who suffer from any lung disease already.

Exercising doesn’t necessarily mean exhausting yourself
For people who have a lung disease, like asthma or COPD, exercising often seems just bridge too far. But exercising does not have to be strenuous. A small research with COPD patients doing mild exercises in a bath filled with warm spring water showed a remarkable reduction of their symptoms and improvement of the condition of their lungs as well as their oxygen saturation. Also special training like yoga or tai chi have seen to be very wholesome for COPD patients, and can even slow down the progression of diseases like emphysema.
For asthma patients, especially those suffering from exercise-induced asthma, a simple exercise as blowing in a bottle regularly, can improve their lung function significantly. This was demonstrated by a research where 212 patients were asked to blow into a bottle every 4 hours, during 4 months. After this period their FEV (Forced Expiratory Volume, which is the amount of air that can be blown out in a one second forced exhalation) showed a stable improvement of their lung function. Apart from that they needed to use their inhalers a lot less during this period. 65-75% of the improvement remained for over half a year, even without blowing in the bottle.
It seems only logical that, if these simple exercises are so beneficial to already damaged lungs, they would be just perfect to keep your still healthy lungs in tip top shape. So don’t wait until it is too late, start exercising and let your lungs absorb the oxygen to energise your body. No need for exhausting exercises, a nice walk in the fresh air, that you can breathe in deeply, is sufficient and may be even the best!
Eat vegetables and fruits to keep your lungs in the best possible condition
More and more scientists and researchers emphasise the importance of eating ample fruit and veggies, around 400 grams daily, to keep our bodies healthy. Specific research has recently shown that especially our lungs also benefit from this kind of diet. A researcher from the section Health & Environment from the University of Washington in Seattle found that frequent consumption of vegetables and fruits reduces the chance to develop COPD or other lung diseases, while for people already suffering from COPD, it improved their lung function significantly. Other research found that eating fruits and vegetables offers protection against lung cancer.
If possible, try to get biological products, as these contain more anti oxidants than the regularly grown vegetables and fruits. Furthermore, the biological varieties contain more polyphenols. Both anti oxidants and polyphenols are known to have anti inflammatory and anti carcinogenic properties.
Ref: Medisch dossier, Sept. 2016; Wikipedia
Rheumatoid Arthritis Also Damages Your Lungs
Rheumatoid arthritis is a well-known disease for causing damage to joints, however the disease can also affect your lungs. It can cause damage to the tissue around the joints as well as your eyes, heart and lungs.

“We call it rheumatoid arthritis, but we should really call it rheumatoid disease,” says Elinor Mody, MD, director of the Brigham and Women’s Hospital Women’s Orthopaedic and Joint Disease Centre in Boston. Besides the joints, the “heart and lungs are the most commonly affected,” Mody says. Doctors aren’t sure how or why rheumatoid arthritis causes other organs to suffer, but lung complications of rheumatoid arthritis can be serious and even cause death.
Interstitial Lung Disease
Rheumatoid arthritis-associated interstitial lung disease, or RA-ILD, is the most serious lung complication for people with rheumatoid arthritis. This illness can be hard to detect, but occurs when lung tissue becomes inflamed and eventually scarred.
* Smoking increases the risk of developing it but non-smokers do develop RA-ILD.
* It causes breathlessness and a dry cough, but in many cases it is symptomless making it difficult to be able to detect it early enough to try and treat it.
* There are trials going on at the moment trialling new drugs to try and treat it but nothing has been very successful so far making the disease difficult to treat, other than treating the symptoms.
Pulmonary Fibrosis
The inflammation and scarring caused by RA-ILD can lead to pulmonary fibrosis and permanent scarring of the lung tissues. The air sacs are gradually replaced by scar tissue reducing the respiratory capability of the lungs and resulting in shortness of breath.
* Supplemental oxygen can be used to help make breathing easier but it cannot reverse the dame done by pulmonary fibrosis.
* Methotrexate is a drug commonly used to treat rheumatoid arthritis, however this drug also causes pulmonary fibrosis. If you are on this drug then your
respiratory status needs to be carefully monitored.
Nodules
Rheumatoid arthritis can also cause nodules to form in the throat and on the vocal cords, causing complications like hoarseness and other changes. Nodules can develop in the lungs as well, but usually don’t cause symptoms and patients may never notice them.
Prevention of Respiratory Issues
Because of the high risk of complications due to rheumatoid arthritis-associated lung disease and the fact that there is little treatment available, prevention is key. To help reduce your risk:
* Don't smoke. If you do, ask your doctor for suggestions about how to quit smoking immediately. Chemicals found in cigarettes can irritate already delicate lung tissue, leading to further complications.
* Have regular check-ups. Your doctor should listen to your lungs and monitor your breathing at each visit as lung problems that are detected early can be easier to treat. Talk to your doctor about any shortness of breath you're experiencing and ask about changing medications or starting supplemental oxygen therapy to help ease symptoms.
References: http://www.everydayhealth.com
Exercise table could help alleviate COPD symptoms
A team of researchers in America have developed and are currently testing out a table that may be able to help patients that suffer from the effects of COPD.

The team consists of people from all disciplines that have come together to pool their knowledge of COPD and patient's pulmonary care and treatment to help these patients to improve their breathing.
The table is based on a gravity-powered approach to improve ventilation as well as helping to clear mucus. The table appears stable but in fact rocks forward and backwards with weight. The person on the exercise table lifts and pulls a bar while rocking the table forward
As the person pushes away the table then rocks backward resulting in the person's feet being higher than their head. This movement forces air out of the lungs, which is normally difficult for a COPD patient to do and therefore reduces the difficulty of breathing for the patient. This approach also uses gravity to help the tiny hairs in the lungs to move the mucus along the trachea as well as the gravity also helping to move the lymphatic fluid out of the lungs. The movement of the abdominal viscera also moves the diaphragm which also reduces the effort of breathing.
The table not only aids the lungs and breathing but also benefits the rest of the body. The gravity effect on the body results in the drainage of lymphatic fluid from the arms and legs, improving circulation and reducing swelling.
One of the founders of the company is himself a COPD sufferer and says that the table has alleviated his symptoms greatly but the table is currently being vigorously tested in trials.
References: http://copdnewstoday.com
Using opioids worsens your COPD
COPD patients are often prescribed opioids such as codeine, oxycodone and morphine to provide relief from common symptoms such as muscoskeletal pain, insomnia and respiratory issues. However it has been shown by researchers in Toronto, Canada that opioids can induce additional respiratory side effects and that new opioid users have 5 times a greater risk of death compared to non-opioid users. These results raise serious safety concerns about the use of opioids for older adults with COPD.
“This is a population that has a chronic lung disease, with symptoms that can sometimes be challenging to manage,” said Dr. Nicholas Vozoris, lead author of the study. “This class of drugs may offer some relief; however, there is also evidence suggesting that opioids can adversely affect breathing and lung health in people who already have chronically compromised lungs.”
Previous studies reported that opioids were safe for patients with advanced COPD but the results were not reliable due to study limitations.
In this new study over 130,000 patient records were examined from multiple healthcare databases to try to ensure the results were more generally applicable and reliable.
“Previous research has shown about three-quarters of older adults with COPD have been prescribed opioids, which is an incredibly high rate of new use in a population that is potentially more sensitive to narcotics,” Vozoris said. “Our new findings show there are not only increased risks for respiratory-related death associated with new opioid use, but also increased risk of visits to emergency rooms, hospitalizations and needing antibiotics or steroid pills.”
The team found that those who used opioids had an increased risk of 14% or ending up in the emergency department and nearly 3 times the risk of COPD or pneumonia-related mortality. They even have an overall mortality risk of 76% compared to non-opioid users. Opioids were however found to decrease the risk of respiratory exacerbations by 12%.
The higher risks were found in patients using stronger or higher dosage opioids however many risks were unaffected by dosage if you were a new user.
Opioids can impact COPD patients in several ways such as respiratory depression, reduced mucous clearance from cough suppression, and immunosuppressive effect.
To lower the risks of adverse events doctors may prescribe less potent or lower dosage opioids but the results of the current study showed increased risk of complications and even death regardless of dose amount among new opioid users. Vosoriz said the finding is important because lower doses were long considered safe.
“Sometimes patients are looking for a quick fix for chronic pain or breathing issues and physicians may believe opioids can offer them some relief,” he added. “The trade-off becomes explaining that there are risks to patients and making sure they understand that potentially alleviating their symptoms could come at a higher cost to their health.”
An individual multi-disciplinary approach is better as a treatment plan rather than just prescribing opioids. Making use of pulmonary rehabilitation, supplemental oxygen therapy, exercise and lifestyle changes in conjunction with medication is best way forward for COPD patients.
References: http://copdnewstoday.com and http://lungdiseasenews.com
Non-pharmacological Treatments for COPD
Despite there being excellent medications for COPD patients, such as bronchodilators which are continually improving in both potency and in delivery there is still a huge proportion of the COPD patient population who continue to experience deterioration in their symptoms and poor quality of life. There are however many non-pharmalogical treatments that can provide huge relief for many patients. They may work alongside your pharmalogical treatment or you may decide that they are better used instead of, but always consult with your doctor.
Smoking cessation is the most important of these. It has been shown and still being proved in continuous research how cigarette smoke harms not just your lungs but also the rest of your body. It the primary cause of COPD and the chemicals have been shown to affect your cells right down to its DNA and causes abnormalities, inflammation and permanent damage which greatly worsens your symptoms and respiratory ability. There are lots of different ways you can be aided in stopping, with patches, gum and electronic cigarettes. Its always best to support your method with counselling or support groups.
Telemedicine allows patients with COPD to connect electronically with a specialized care consultant. Telemedicine can be used to collect information from the patient and track his or her progress on a daily basis, if necessary. It has been used to alert the medical team to the early onset of acute exacerbation of COPD thereby avoiding emergency department visits and hospital admissions. However, more evidence is needed as some studies state that "telemonitoring for COPD is not yet proven and further work is required." There are many devices already out in the market which are easy to use and allows the user to feel more in control and to monitor their respiratory vitals on a daily basis and adjust their regime quickly when alerted to avoid unnecessary attacks and deterioration.
Pulmonary rehabilitation is important in order to sustain your mobility and quality of life. It aims to counteract the loss of skeletal muscle that is common in COPD and to improve exercise tolerance. There are a variety of methods including exercise training, nutritional supplementation, and psychosocial support. Although it is not yet proven to have direct links to increased survival or lung function, there have been improvements in health-related quality of life, dyspnea, and exercise tolerance. There has also been a tendency for any accumulated improvements to deteriorate with time unless the methods are continued.
Long-term oxygen therapy is also an option for some patients with COPD. Short-term use of oxygen during exercise or strenuous activities in patients with any degree of hypoxemia has long been known to improve dyspnea and increase exercise tolerance, although is not proven to extend survival. For patients who are chronically hypoxemic long-term oxygen therapy where the patient uses it constantly through the day, not only improves exercise performance and quality of life but also improves survival rates. There are many different devices depending upon your lifestyle and requirements and can be obtained via the NHS or from private companies. They are much more compact, lightweight, discrete and portable than ever and still allows the patient to move around easily both in their home and outdoors so as to allow the patient to have a significantly increased quality of life and eliviate respiratory symptoms.
Noninvasive positive pressure ventilation (NIV) has been effective when treating COPD patients that suffer from acute exacerbations. Gas exchange and respiratory abilityes are improved, resulting in decreases in intubation rates, shortening hospitalizations, and improving mortality. However, its long-term role in managing COPD has not been demonstrated and its unclear as to whether nocturnal NIV will signoificantly improve lung function, gas exchange, or sleep efficiency.
Patients with severe emphysema typically have bullae. These are growing air spaces that occupy space within the thorax but do not provide much gas exchange. They are more likely to impair the function of less diseased lungs by occupying dead space within the thorax and contributing to air trapping and ventilation/perfusion problems. The aim of surgical lung volume reduction is to remove nonfunctional lung and thus improve lung physiology and symptoms. A large study showed that this treatment is only truely beneficial to patients with predominantly upper lobe disease and low prior exercise tolerance. Other subjects tended to have higher mortality. The procedure is rarely performed today, but there are attempts to achieve a similar outcome, by less invasive methods. These employ the placement of one-way valves in the lung airways that allow gas to leave bullae but not return. The valves are placed bronchoscopically into the lungs. In general, some improvement in lung function, less dyspnea, and improvements in exercise capacity have been obtained, but there has usually been an increase in adverse effects, including acute exacerbations of COPD and pneumothorax, sometimes requiring removal of the valve(s). Lung coils are another method proven to be very succesful. Doctors insert special flexible scopes through the patient’s mouth to place metal coils into the damaged tissue of the patient’s lung. The coils return elasticity to the diseased tissue, allowing the lungs to work in a more normal way. Other experimental lung procedures with the same aim have attempted to collapse the most emphysematous lung regions by closing the airways to those regions by other means, but development of these methods is incomplete.
Lung transplantation has been an option for patients with severe COPD since 2000, with 50% survival being in the region of 5 years and steadily improving. It should be considered only in patients with end-stage COPD, only when all other therapies have been tried and failed to provide relief. Primary graft failure, chronic rejection, and infection are common problems, however, there can be successes where lung function and quality of life can markedly improve, and outcomes are improving with time.
References: www.medscape.com
Cigarette smoke affects your DNA
A recent study proposed the idea that damage to our DNA at the telomeres contributes to lung ageing, continuing damage and worsening COPD symptoms. Also that cigarette smoke increases and encourages such damage to the telomeres.

Telomeres are specialized structures at the ends of chromosomes within our DNA that protect it from deterioration and prevent fusing with nearby chromosomes. COPD has long been associated with accelerated lung aging and abnormal cell division. Telomeres shorten with each cell division, therefore the more the cell divides the less protection the DNA strands have.
In a newer study they investigated telomere dysfunction in lung airway cells from patients with COPD using lung aging mouse models exposed to cigarette smoke. They found that there was no difference in telomere length between control patients and COPD patients, which contradicts the previous study although they say that this could be due to a small sample size and will need to be repeated with a larger amount of samples.
With age they observed an increase in telomere dysfunction and that this was also increased with exposure to cigarette smoke. They found that the cigarette smoke accelerated the telomere dysfunction by increasing levels of reactive oxygen species (free radicals) and aided in the secretion of inflammatory cytokines.
As a result, the team highlighted that their findings suggest that telomeres are particularly susceptible to damage triggered by cigarette smoke, and that this may lead to an accelerated decline of lung function in both aging and COPD patients. So whether you have COPD or have normal respiratory health, exposure to cigarette smoke will trigger telomere dysfunction, affecting the DNA within the cells and causing damage to the cells in your lungs. And thereby reducing respiratory function in the elderly and worsening symptoms in COPD patients. This study suggests that the elderly and patients suffering from respiratory illness should not only stop smoking but also not be around other smokers in order to preserve their respiratory health.
References: http://copdnewstoday.com
Possible cure for PAM and other rare lung diseases?
Pulmonary Alveolar Microlithiasis (PAM) is a rare lung disorder where small stones form and accumulate in the air sacs of the lung. These stones cause inflammation, scarring of lung tissue and reduced respiratory ability resulting in the patient requiring supplemental oxygen.
New research from a team at the University of Cincinnati has uncovered and identified key bio-markers and a potential new therapeutic approach that could be the key in treating this rare lung disease.
A few years ago a team discovered that DNA mutations in the gene SLC34A2 caused a loss of a cellular pump which would normally remove phosphate from the air spaces in the lungs. As a result calcium and phosphate levels rise in the alveolar sacs and cause the formation of stones or microliths that invoke inflammation. Patients find that by middle-age this chronic inflammation has caused scarring and damage to the lungs and experience respiratory failure.
The team collected samples from people all over the world with help from the RDCRN programme who's goals are to advance medical research on rare diseases by providing support for clinical studies and to facilitate collaboration and data sharing. This enables scientists from multiple disciplines at hundreds of clinical sites around the world to work together to help study more than 200 rare diseases.
They found that those with mutations in this specific gene also had elevated levels of certain serum markers. Certain cytokines and surfactant proteins were raised in line with the presence of stones in the lung, suggesting that by testing and monitoring these levels it could be a useful tool in following the disease progression and treatment responses in patients.
They also discovered that the stones dissolved easily in EDTA, a molecule used in many detergents as it binds to calcium. "Washing the lungs with an EDTA-containing solution reduced the burden of stones in air spaces," says Dr McCormack. "This finding could translate into a therapy for humans if toxicity studies demonstrate that the approach is safe."
A low-phosphate diet was found to prevent stone development and to even reverse lung calcification. However low phosphate levels can cause other medical problems and this approach will need to be tested in clinical trials first. Although another strategy is to utilise gene therapy and to insert a gene for a working phosphate pump back into the cells using viral vectors.
"This study demonstrates how discovering the causes of these rare lung diseases not only can inform us how the lung normally functions, but can also lead us to potential therapeutic interventions for these rare and often lethal lung diseases," says James Kiley, PhD, Director of the Division of Lung Diseases at NHLBI.
McCormack says rare disease research can reveal surprising insights into the fundamental biology of the lung. "Studies of the PAM.. model have already revealed a potential role for phosphate in the regulation of surfactant balance in the lung and have attracted the interest of cystic fibrosis scientists interested in exploring the possible interaction between [the phosphate pump] and the defective chloride channel in that disease," explains McCormack.
Although human trials are a few years way, UC's research offers some hope to patients who suffer from this rare disease. Kathleen Falco, 65 from Riverhead in America shares a similar story with other patients. She was misdiagnosed with Sarcoidosis in 1977 until 2000 when they diagnosed PAM. It started to take its toll in her 40's and a few years ago her symptoms intensified and she has shortness of breath, reduced mobility and dependency on supplemental oxygen. She cant walk, take part in outdoor activities, has lost weight and finds it hard to breathe when its hot or cold. She felt isolated, with little information and no support network or forums and eventually sort out help through the internet and was put into contact with Dr McCormack. She's hoping that the trials will be a success and that she may be able to live out her retirement years being able to breathe a bit easier and enjoy a much improved quality of life.
References: http://medicalxpress.com and https://www.sciencedaily.com
Asthma can reduce your productivity
A new survey has shown that 75% of people who suffer with asthma blame their illness for a significant reduction in productivity at work and asthma patients on average miss 3 hours of work a week due to their illness. The survey also showed how patients are also feeling that they have a lack of productivity when it comes to household chores and daily activities as well as at work.

All 1,598 patients surveyed were taking their prescribed medications and were from various countries. 74% reported issues around productivity at work and also 3 hours of work missed a week. 9% reported a complete inability to work and 67% reported sleep disturbances.
The survey was conducted by the Think.Act.Breathe campaign who help asthma patients identify personal risk and improve immediate and long-term risk of asthma exacerbations.
Dr. Kevin Gruffydd-Jones, lead author of the report said the findings illustrate how asthma can impact a patient’s economic burden, even while on medication.
“People with asthma often accept their symptoms and the impact they have on their daily lives. It is important that people with asthma talk to their doctor about how their asthma is affecting them at work, their sleep and daily life, and to discuss what more could be done to help them feel better and live life to the full.”
Asthma may cause physical and mental affects as well as the obvious physical ones and can have an impact on your whole life. Only 13% reported no impact on their work but 23% reported feeling tired and weak at work as well as 18% feeling mentally strained. 51% also stated that their symptoms had a negative impact upon their ability to complete daily chores outside of work.
“Asthma affects millions of people worldwide and most people with asthma have low expectations of what can be achieved by asthma management and don’t realise that their condition can be improved,” said Boehringer Ingelheim’s Head of Respiratory Medicine.
Many people get an initial diagnosis and treatment but never go back to the doctors for a check-up. However symptoms change and science moves forward and it is important to go back to your doctor regularly especially if symptoms lessen or worsen. New drugs, new treatment methods, breathing techniques and supplemental oxygen among other things could be available to you to help to improve your quality of life, reduce the frequency of exacerbations and lessen symptoms. Sleep disturbances could be due to sleep apnoea which could be eased with supplemental oxygen and a slight change to your treatment could greatly improve your oxygen levels, sleep and breathing which would greatly improve your productivity at work and at home.
References: http://lungdiseasenews.com