Injected biosensors could measure your oxygen levels
A company in California has invented biosensors that can be injected into the body and not be rejected by the body's immune system. They could well replace traditional clinical laboratory testing and make our bodies continually accessible 24/7 so that we know exactly whats going on in our bodies and improve our health. The capability for these new biosensors to provide long-term, continuous streams of live data about the levels of various molecules in our body could completely alter the relationship we have with our bodies as well as transforming the healthcare system.
We rarely get the chance to see whats happening inside our body unless we see an x-ray or have specific tests done; we rely on our doctors to take some blood or perform other one-ff tests in order to get a single snap shot of whats going on and interpreting it for us.
If we could see the data for ourselves continuously in real time, then we can make timely choices to prevent symptoms getting worse and have a continuous conversation with our own bodies to keep it within healthy parameters.
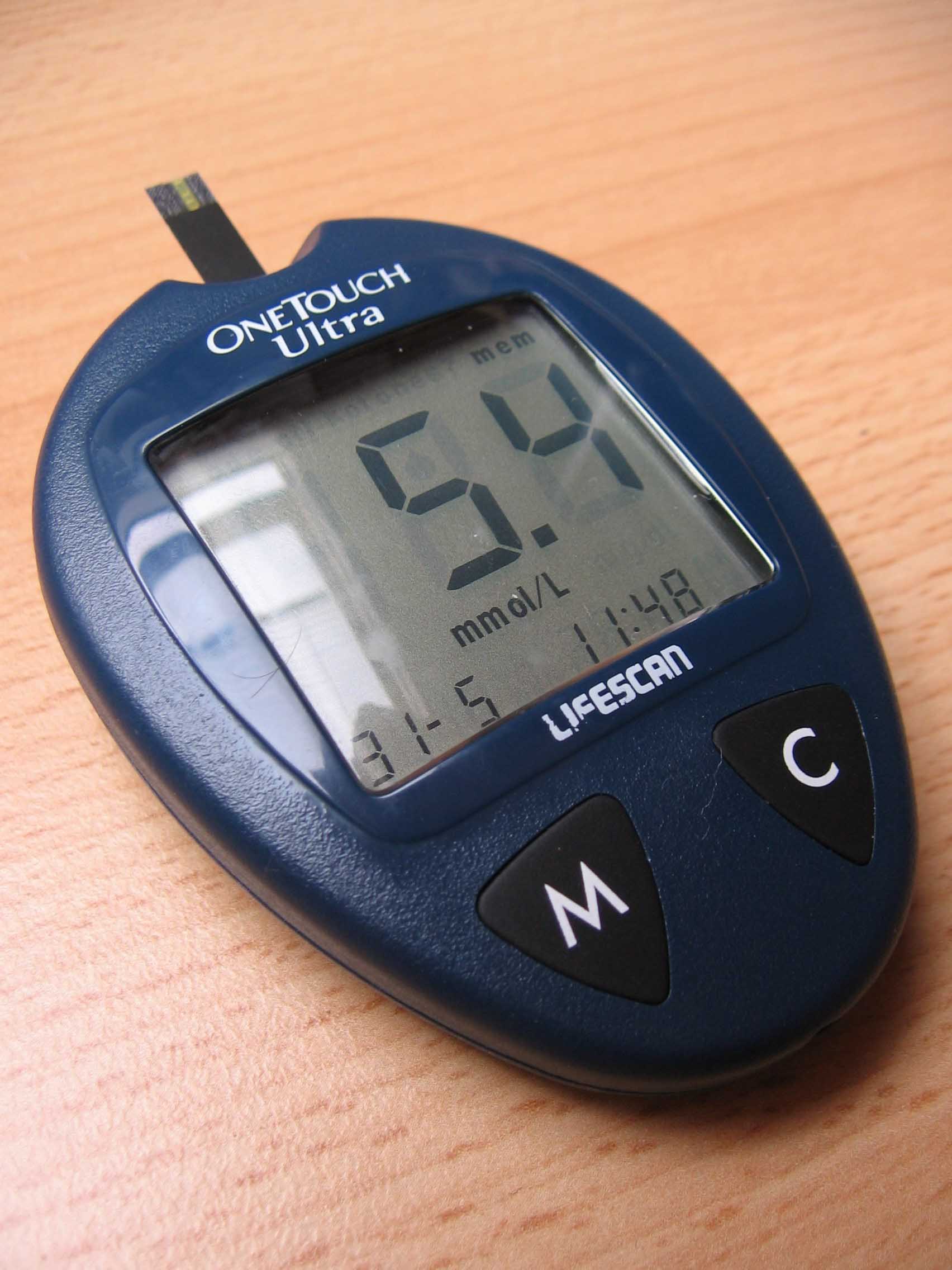
These new biosensors will have uses not only for healthy individuals wishing to remain so and monitor their health and fitness but also could be used in the management of chronic diseases such as diabetes and COPD.
"Our tissue-integrated biosensor technology meets three key criteria for continuous monitoring: First, the data needs to be clinical-grade so that you and your healthcare provider can make medical decisions about your health and wellbeing. Second, the user experience needs to be seamless so adoption can fit into any workflow environment. And finally, the technology needs to be accessible at a reasonable cost in a form function that's easy to use," explained Dr Hwang.
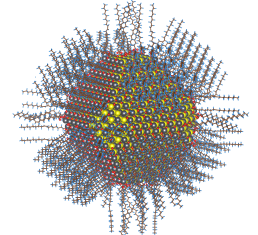
The biggest hurdle of biosensor development has been how to overcome the effects of the foreign body response and to stop the body from rejecting what it thinks are foreign objects. The biosensors are placed under the skin with a specially designed injector. Each biosensor is a flexible fibre of 3-5mm long and 500 microns in diameter. Rather than being isolated from the body these sensors are fully integrated into the tissue of the body. There are no metal devices or electronics involved and therefore overcomes the effect of the foreign body response.
Each biosensor is comprised of a bio-engineered 'smart hydrogel' which is similar to contact lens material which forms a porous, tissue-integrating scaffold that also induces blood vessel growth and cell growth in the surrounding tissue. The smart gel is linked to a florescent light-emitting molecule that continuously signals the presence of a body chemical like oxygen or glucose.
Adhered to the skin's surface or held by hand, a separate optical reader is used to read the fluorescent signal from the embedded biosensor. The reader sends excitation signals through the skin to the biosensor, which then emits light proportional to the concentration of molecules being tracked. The data can be relayed to a smart phone for an encrypted personal record and historical tracking.
Their oxygen sensing system that the company has developed is a single biomarker sensor designed to measure dissolved oxygen in the tissue. It is the only long-term monitoring technology that guides therapeutic action and measures tissue oxygen levels during the treatment and healing process for peripheral artery disease (PAD). It will be available in Europe this year to be used by vascular surgeons and wound-healing specialists. Other respiratory disease patients can also benefit from using this technology such as those who suffer with COPD. They can continuously measure their oxygen levels using real time data in order to be able to adapt and alter medications and supplemental oxygen flow rates in order to prevent exacerbations and hospital admissions. It would help respiratory disease patients to continuously monitor their condition and provide real data for their healthcare provider to monitor and aid in their long-term treatment. It could help prevent exacerbations and help to prolong quality of life and increase survival rates.
In the future we would be able to monitor practically every biomarker in our body and would not need blood tests and some other clinical monitoring tests at hospital to be performed and would reduce the burden upon on the healthcare system. Results could be sent wirelessly to the doctor who could monitor from afar and would change the way medicine is practiced and put the responsibility and control into the hands of the patient.
References: http://www.prnewswire.com
Man's best friend could help with your mobility 24/7
For many people with a lung disease like COPD it can become so restrictive and isolating. Many people get to a stage in their condition where they require oxygen 24/7, which means they are linked to an oxygen canister via tubing permanently, greatly restricting their mobility. It can result in people not wanting to go outside or exercise due to having to deal with the hassle of tubing and concentrators and feeling conspicuous. It is especially difficult for children that have respiratory problems who would normally want to run around and play games.

A child in America has a rare lung disease and she has a specially-trained dog who has been with her since she was little. He carries her oxygen concentrator around and always ensures he doesn't tangle up the tubing and stays within a certain proximity to her. This has meant that not only does the child have a long-term companion to help prevent the feeling of being alone caused by long-term illness, but also allows the child to go out and about, play, exercise and go to school more easily which benefits their health and social development.
This idea of an 'oxygen dog' could be rolled out to people of all ages who require assistance, especially those who are elderly, alone and finding it difficult to cope and get out and about due to their need for 24/7 oxygen. A smaller dog could only carry a portable concentrator however a larger dog would be able to carry a small oxygen tank.
The benefits of having the dog as a puppy when the child is also young is that they can grow and develop together. Different lung diseases at different stages will affect the individual differently so having the dog training at a young age with the patient means that the dog can learn how to deal with different situations and develop with the owner and know how to assist them better and predict movement based on behaviour patterns.
Having a dog is not cheap however and is by no means about to become readily available via the NHS, however it is an avenue that some people may be able to afford or raise funds for as a way to help them enjoy a better quality of life.
References: http://www.stuff.co.nz
Vikings and worms provide clues to the cause of COPD
Revealing Viking Genetics and COPD
Scientists have found evidence that the Vikings may have carried a genetic defect that causes Chronic Obstructive Pulmonary Disease (COPD). According to archaeological digs in Denmark, Viking communities experienced significant worm infestations, which had an impact on their genetic evolution. Although useful in the past, this adaptation is currently associated with a higher risk of COPD.
COPD and the Viking Legacy
The condition known as COPD, which impacts around 5% of the world's population, is greatly impacted by a hereditary alpha-1-antitrypsin (A1AT) deficiency. Due to the evolution of this genetic feature over 2,000 years ago in Viking tribes, it is especially common in Scandinavia.
The protein A1AT shields the liver and lungs, among other important organs, from the protease enzyme. If not controlled, these enzymes—which are made by parasitic worms and the immune system—can seriously harm tissue. COPD is caused by these proteases dissolving lung tissue due to an A1AT deficiency.
Historical Appropriation and Modern Day Consequences
According to Professor Richard Pleass, the Viking diet, which was frequently tainted with parasites, caused their bodies to change. Originally, the aberrant versions of A1AT served as a defence against these parasites, but they now raise the risk of COPD. These variants attach to Immunoglobulin E (IgE), an antibody that worm proteases cannot break down, protecting the Vikings' critical organs.
"In ancient times, these deviant forms of A1AT were crucial for survival against parasitic infections," according to Professor Pleass. "However, with the advent of modern medicine and the eradication of many parasitic diseases, these genetic traits have become a liability, contributing to the development of COPD."
Genetics Today
This finding clarifies why A1AT deficiency still exists in some populations. It implies that if you are of Viking descent, you may be genetically predisposed to COPD, particularly if you smoke or live longer than the Vikings did.
A1AT deficiency's evolutionary history demonstrates how a genetic adaptation that was advantageous in one era can turn out to be harmful in another. This historical viewpoint emphasises the need of knowing our genetic ancestry and offers insightful information about the genetic components of COPD.
The ways that ancient adaptations still affect our health today become more evident as we learn more about our genetic heritage. Knowing the Viking roots of A1AT deficiency sheds light on COPD and emphasises the value of genetic research in the fight against contemporary illnesses.
References
A machine that can help to repair lungs to make them transplant viable
A machine has been developed that can recondition a set of lungs outside of the body in order for them to improve and make them healthier ready for transplant into a recipient. The machine is known as 'the box' and it ventilates lungs after their removal from the donor. It also infuses them with a mix of fluid, drugs and steroids which allows the lungs to dry out and get them into a better shape before being transplanted.
"It allows the lungs to stay alive... and allows us as providers to assess the function of the organ in a unique, well-controlled environment," said Dr. Varun Puri.
The machine is made up of a ventilator to help simulate breathing and a bypass machine to perfuse the lungs with drugs and fluid In order to improve their function and generally helps to mimic the body with one major helpful difference. The lungs normally undergo a lot of stress in the body constantly exchanging gases with every breath, however in this box that stress factor is removed and gives the lungs a chance to heal.
This machine will hopefully help to improve lung transplant statistics and aid in improving the long-term survival rates of those that suffer from respiratory diseases like COPD. Currently fewer than 20% of donor lungs are considered suitable for transplant and 25% of candidates dies whilst waiting for a transplant. Even the survival rate post-transplant is 50% to survive 5 years. This device could aid in increasing the donor pool as the machine can take lungs that were previously deemed as unsuitable and give them a chance to heal and improve, making them then viable lungs for transplantation. With more lungs available for transplant fewer patients will die waiting and if the lungs are healthier when transplanted then hopefully the survival rates for lung transplants will also improve with further research.
“I am sure in the future we will be able to do things like gene therapy to the lungs in a controlled environment or utilizing specific anti-inflammatory agents to prevent short term and long term rejection of organs.” said Dr. Varun Puri.
Michele Coleman, 63, credits 'the box' with saving her life. A former smoker, she was diagnosed with chronic obstructive pulmonary disease and doctors asked if she would participate in a clinical trial.
"You don't want to, but you kind of lose hope because when you are sick like that you know how fast you are going downhill," Coleman said. "It's scary, but anything that they could give me was going to be better than I had, and actually I figured I wouldn't make it to the end of the year," she said. The transplant for her was a huge success and she is still doing well with her 'reconditioned' lungs.
There is also hope of being able to do the same with other organs to improve transplantation survival rates across the board. Hopefully 'the box' brings a little light to those with severe respiratory diseases where their lungs are failing them.
References: http://www.foxnews.com and http://www.trunews.com
Nanoparticles can break through the mucus barrier
A team of experts in Brazil have demonstrated how their recently designed DNA-loaded nanoparticles are capable of passing through the mucus barrier in the lungs.
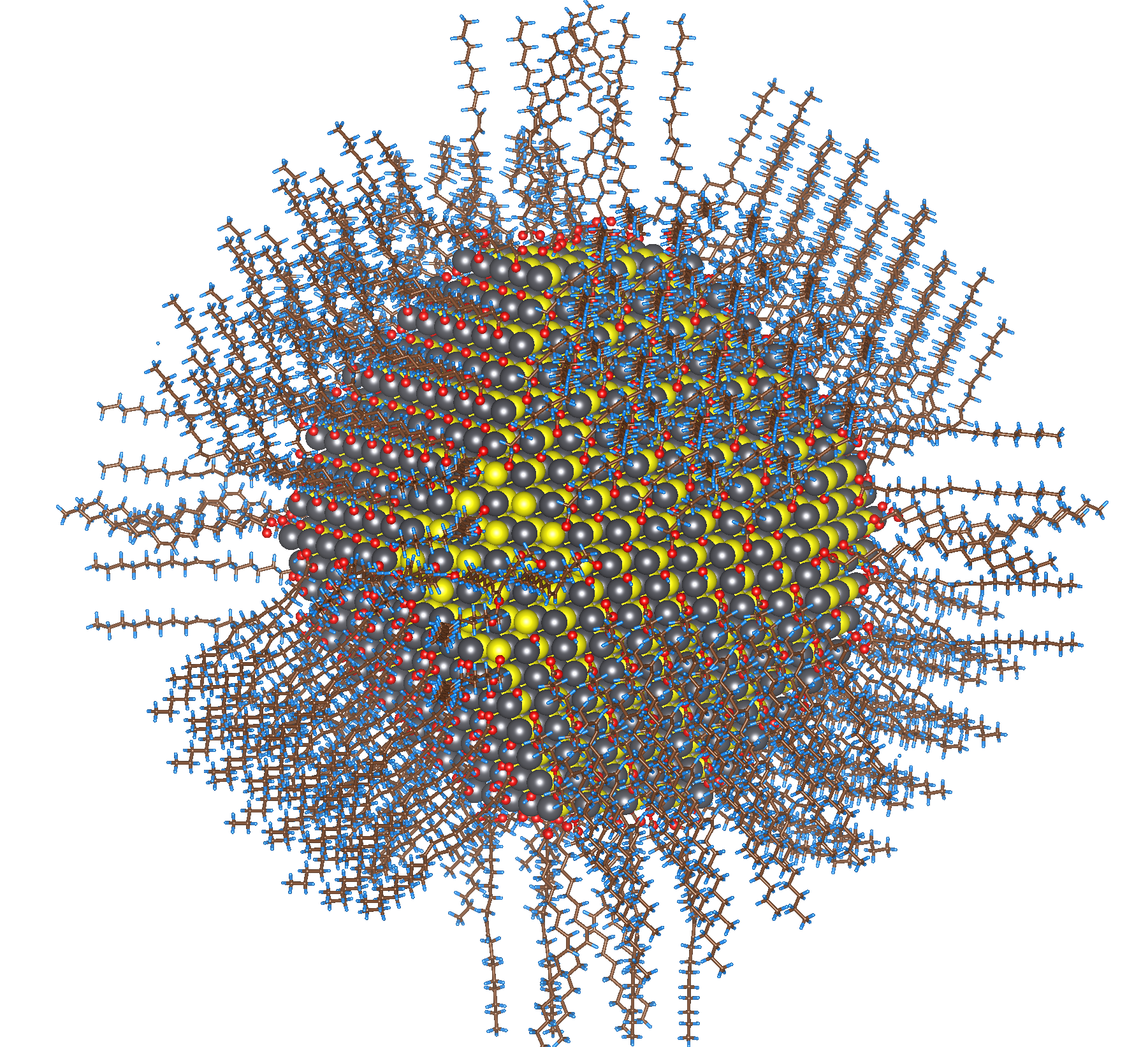
They believe that this can potentially lead to the development of therapeutic genes that can be delivered directly to the lungs using the nanoparticles to help treat CF, COPD and asthma.
“To our knowledge, this is the first biodegradable gene delivery system that efficiently penetrates the human airway mucus barrier of lung tissue,” said study author Jung Soo Suk.
The lung's mucus barrier is important to keep lungs healthy as it is responsible for protecting the lungs from being infected by bacteria and foreign agents. The inhaled particles are trapped in the mucus and swept away from the lungs via beating cilia and goes to the stomach to be degraded. In many respiratory conditions this mucus barrier is a lot thicker and drugs cannot penetrate the barrier to get to the damaged cells underneath it and blocks treatment.
The team worked to demonstrate that by placing replacement or corrective genes or drug agents inside a biodegradable nanoparticle 'wrapper' that these can be inhaled by the patient and are able to pass through the barrier and work to correct defective genes within lung tissue cells in order to correct these cells so that they work more efficiently and significantly improve respiratory conditions. This would be excellent treatment for severe lung diseases as it would be efficient, a unique dose could work for many months and there would be less adverse side effects and no lung inflammation.
Previous studies have shown that non-viral, DNA-loaded nanoparticles have a positive charge which causes the gene to become attracted to and stick to the negatively charged mucus within the lungs. This has prevented traditional nanoparticles from effectively making it to their targets as they keep sticking to other unwanted targets during the journey through the lungs and also tend to aggregate and clump together making them too large to penetrate the mucus.
The new nanoparticles have a dense coat of a polymer called PEG, which neutralises the charge and prevents the sticky exterior problem. The study showed that these newly designed nanoparticles keep their size and rapidly penetrate the mucus layer. They are also biodegradable containing a protein which breaks down the delivery system once it has delivered its contents to the lung tissue cells.
They are now planning to move on to studies with humans and hopefully this potentially highly effective treatment wont be too many years away. It also demonstrates how wide-ranging the nanoparticle delivery system could potentially be and that by tweaking the system depending on the environment, the method could be used to effectively administer drug treatments to all areas of the body that previously had been considered difficult to reach or with barriers preventing drug access.
References: http://copdnewstoday.com
New device could predict asthma attacks in children

Researchers from a University in Utah have developed a model that can anticipate the deterioration of asthma in children. Asthma is a chronic inflammatory disease where the airways narrow and become swollen due to mucus accumulation in the lungs. Patients experience difficulty in breathing, coughing, frequent respiratory infections and tightness of the chest. It is believed that asthma is caused by a combination of genetic and environmental factors such as pollution, dust and smoking. There is no cure for asthma, for those with mild cases it can be handled by avoiding triggers such as pollution and certain foods but for those with more severe cases medications are needed to try and treat the symptoms however many patients suffer more frequent exacerbations and asthma attacks. Oxygen therapy and more severe medications are also sometimes needed for those that suffer from it badly.
Millions of people suffer from asthma and children are affected more than adults. Asthma attacks can be terrifying for both the child and their parents and it is difficult for a child to communicate their health status. Sometimes the parent has no idea the child is unwell until they cant breath and are in the middle of an asthma attack. This also results in huge cost to the NHS with children being admitted to hospital after visiting the A and E department for an attack. It would be helpful if the child or parents could anticipate that an attack may occur so that they can be prepared and maybe put into action a plan to prevent an exacerbation or reduce the frequency or severity of them.
The researchers have developed a machine learning model that is able to predict signs of asthma deterioration in children one week prior to an exacerbation. The Asthma Symptom Tracker is a self-monitoring tool that has been trialed on children with asthma over a 2 year period. The data has been collected and allowances made for temperature, humidity, tree pollen count etc and the results suggested that the mode; was 71% accurate, 74% sensitive and 71% specific in predicting an exacerbation a week later.
This model can now be integrated into an electronic device, which can be worn by the user. The device can take constant readings and warn the user of a potential case of deterioration in their health. The overall success rate is around 75% so would be extremely useful in helping those that suffer from asthma, as hopefully in the future a model can be developed for adults too. This could reduce exacerbations, improve the well-being of the patients and decrease the burden on the health care system.
References: http://lungdiseasenews.com
Oxxiom - The World's First Wireless and Fully Disposable Pulse Oximeter
The company 'True Wearables' based in California has launched a new product called 'Oxxiom', which the company claims to be the world's first wireless and fully disposable, single-use pulse oximeter.

Pulse oximetry technology is a non-invasive method of monitoring a patient's pulse rate and oxygen levels, which provides your doctor with an indication of your real-time cardio-respiratory status. They are widely used during medical procedures, during sleep monitoring and to help monitor conditions such as COPD, heart attacks and sleep apneoa. The principle of pulse oximetry is based on the red and infrared light absorption rates of hemoglobin. Oxygenated hemoglobin absorbs more infrared light and allows more red light to pass through, while deoxygenated hemoglobin absorbs more red light and allows more infrared light to pass through. Pulse oximetry uses a light emitter with red and infrared LEDs that shines through a site with good blood flow that has fairly translucent skin such as the finger, toe, or lobe of the ear. Opposite the emitter is a photodetector that receives the light that passes through the measuring site.
The Oxxiom is a small, feather-light, compact and user-friendly device which literally fits on the tip of your finger. It is packed full of electronics and bio-sensing technology but is completely wireless and provides over 24 hours of continuous pulse rate monitoring equivalent to the technology found in hospital. Its disposability eliminates the issue of sterilization and reduces the risk of cross-contamination so can be used in a clinical setting and each patient can get a fresh device or if used at home it is cheap enough for the patient to be able to use a new one every 24 hours. It allows for complete user mobility as it allows the user to sleep in any position, exercise, use the bathroom and shower, whilst still connected to the device. It is also designed to work with any mobile device such as a mobile phone, tablet or laptop and a desktop computer and it does not require batteries or charging prior to use. Also things like nail polish and bright sunshine does not affect the readings, as with other devices. It is simple to use, just pop it on your finger and get on with your daily tasks and forget you're even wearing it. The continuous monitoring provides a detailed record of your cardio-respiratory system and shows how it reacts to different stresses such as exercise. The patient can monitor their own readings and adjust their lifestyle, exercise, oxygen therapy or medication accordingly and the doctor can review the data to provide advice and adjustment of medications or oxygen flow rate as appropriate rather than just basing it on a snap-shot reading at the surgery and the patient's feedback.
The device is due to ship out by the end of the year and soon your monitoring of your pulse rate and oxygen saturation will be a lot easier and more accurate than previously. Its another piece of technology among many that are starting to be manufactured that allow not only for more accurate, in-depth and continuous readings but the user-friendly aspect and the use of apps allows the patient to take more control and responsibility for their own health but also allows a quicker response when health starts to take a turn for the worse and may in the long-term help save lives.
References: http://lungdiseasenews.com
Vegetables can help you breathe easy
Lung disease kills over 60,000 British people every year, with Lung cancer, COPD and asthma being the biggest killers. A healthy diet can slow the damaging effects of smoking and prevent lung cancer from spreading. Lung cancer and COPD are mostly caused by the effects of smoking but a healthy diet of fruit and vegetables may help to prevent the DNA-damaging effects of tobacco smoke as well as helping to prevent cancer from spreading, slow down the progression of COPD and improve lung function. Tobacco smoke contains chemicals that weaken the body's immune system, making it more susceptible to disease and handicapping its ability to destroy cancer cells. But the smoke can also damage cell DNA, increasing the chance of cancer cells forming and flourishing in the first place.

WALK YOUR WAY TO A LONGER LIFE:
The government recommends 150 minutes of moderate activity a week or 75 minutes of vigorous activity spread across the week plus exercise to improve muscle strength at least twice a week.
Walking for 150 minutes a week reduces your mortality rate by 7% compared to being sedentary. Walking for 300 minutes a week reduces it by 14% and an hour-long walk each day reduces it by 24%.
THE POWER OF BROCCOLI:
Researchers asked some long-term smokers to eat a single stalk of broccoli a day. It was found that they suffered 41% fewer DNA mutations during the study. Compounds in broccoli also have the potential to suppress the spread of cancer by preventing the cancer cells from grouping-up together.
THE FEAR OF FRYING:
It is thought that a quarter of lung cancer cases may be caused by carcinogens in the fumes when you are frying. When any fat is heated to frying temperature toxic chemicals are released, which can cause genetic mutations. A study of women in China found that smokers who stir-fried meat every day had nearly three times the odds of lung cancer compared with smokers who stir-fried non-meat foods.
The fumes produced by frying bacon contain carcinogens called nitrosamines. Though all meat may release potentially carcinogenic fumes, processed meat such as bacon may be the worst. A study found bacon fumes cause four times more DNA mutations than the fumes from beef burgers fried at similar temperatures. If you must fry, use a barbecue. Studies show that the number of particles deposited into the lungs increases tenfold when frying indoors as opposed to outdoors.
EATING KALE IS AS GOOD AS RUNNING:
Researchers asked men with high cholesterol to take 3 shots of kale juice a day for 3 months and the kale lowered their bad cholesterol (LDL) and boosted their good cholesterol levels (HDL) to the same levels as if they had run 300 miles. It also increased the levels of antioxidants in the subject's blood. Except in the smoking group as cigarettes create free radicals which counteract this and deplete the body of antioxidants.
MEAT VS VEGETABLES:
One study has found that consumption of cured meat such as bacon, ham, sausage and salami may increase the risk of COPD due to the nitrate preservatives in meat.
In 2010 another study monitored 2 groups; one group kept their normal diet and the other group boosted their fruit and vegetable consumption. Over the next couple of years the first group found that their COPD grew progressively worse whereas the second group found that their disease progression was halted and their lung function had improved. The researchers suggested this could be due to the antioxidant and anti-inflammatory effects of the fruit and veg, along with a reduced consumption of meat, which is thought to act as a pro-oxidant.
TACKLING ASTHMA
A study of more than 100,000 adults in India found that those who consumed meat daily, or even occasionally, were more likely to suffer from asthma than those who excluded meat and eggs from their diets altogether. Researchers removed fruits and vegetables from asthma patients' diets to see what would happen and within two weeks their symptoms worsened. In contrast when they increased fruit and vegetable consumption to seven servings a day the subjects' exacerbation rate halved.
Researchers in Sweden decided to test out a plant-based diet on a group of 35 severe asthmatics who weren't getting better despite the best medical therapies. Of the 24 patients who stuck with the plant-based diet, 70% improved considerably after four months and 90% improved within a year.
From all the studies being carried out, all the evidence seems to point to the fact that a plant-based diet is immensely good for you, if you have lung conditions such as cancer, COPD and asthma and that potentially reducing meat and egg consumption may also be beneficial to your health and aid in halting disease progression, reducing exacerbations, improving lung function and preventing the spread of cancer.
References: www.dailymail.co.uk
Avoiding a lung infection may have become easier with new drug
Many COPD patients suffer from acute exacerbations where their symptoms suddenly get a lot worse and can result in hospitalisation. 75% of the time it is due to a lung infection whether bacterial or viral. The most common culprits are the influenza virus and Streptociccus pneumoniae, which cause the flu and pneumonia.
Bacteria and viruses cause infections in different parts of the lung and cause bronchitis if it occurs in the larger bronchial tubes or cause bronchiolitis if in the smaller bronchial tubes. An infection in the alveoli or air sacs of the lungs can cause pneumonia. Antibiotics are only effective against bacterial infections and viruses are more difficult to treat. Often a patient will acquire a secondary bacterial infection from having a viral one. This is due to the build up of mucus and inflammation in the lungs which create the perfect breeding ground for bacteria. This is why antibiotics are normally prescribed whether the infection is viral or bacterial as to protect from a secondary bacterial infection from occurring.
The other common causes of exacerbations are sinus infections, air pollution, heat failure and blood clots. It is so important that COPD patients try to avoid any of these triggers and try to prevent picking up any viruses or bacteria in order to prevent exacerbations.
The disease compromises the lung's ability to defend against bacteria and a new study has shown that even when a patient isn’t experiencing an exacerbation, the bacteria that are colonized in their lungs are causing respiratory symptoms for them. Having bacteria in the lungs increases the inflammation and significantly increases the shortness of breath, cough and sputum in COPD patients. Doctors are aware that most stable patients experience daily fluctuations in respiratory symptoms but the reason why has never been understood until now. These fluctuations can sometimes be fairly intense and often qualify as exacerbations but go unreported to their doctor.
The study shows that medicine needs to alter its approach to treating stable COPD patients and not to focus on just the flare-ups but to understand that COPD is based around a chronic infection and treat accordingly.
“The lungs are constantly being exposed to microbes ‘with every breath you take’ as well as from aspiration of small amounts of secretions from the throat, especially during sleep,” Dr Sethi says. “If the persistence of these bacteria contributes to increased symptoms and inflammation in the lungs in stable COPD, we should regard this as a chronic infection, not innocuous colonization. For that reason, more must be done to reduce chronic infections in COPD.”
However due to resistance, long-term antibiotic treatment is not the way forward and “we need to put more emphasis on developing therapies that can decrease bacterial colonization in COPD.”
At the end of last year a company announced that the drug AB569 had been successful in trials and appears to be able to treat lung infections caused by Pseudomonas aeruginosa, a common culprit of lung infections in COPD and CF patients. This bacteria is common however it is also difficult to treat as it survives without oxygen and it has the ability to develop resistance against antibiotics as it holds a lot of resistant genes. It causes 40% of infections in children with CF and up to 75% of cases in adults with CF as well as a high percentage of COPD infections. If this drug can treat this bacteria and passes human trials then perhaps it can be used to help dramatically cut the number of infections and the resulting exacerbations suffered by COPD and CF patients and also ease their daily fluctuations of respiratory distress.
Here are eight tips that can help you reduce your risk of developing an infection:
- Wash your hands. Regular hand-washing is one of the most important things you can do to reduce your risk of infection.
- Avoid infections. Ask people who are sick not to visit until they are well again, and wear a face mask if you do have to come in contact with someone who has an infection.
- Clear your airways. It is important to keep airways free from mucus. Your doctor can give you devices and teach you manoeuvres to ensure your coughing is productive at shifting the mucus.
- Stay hydrated.
- Clean your equipment. All equipment that you use, including humidifiers, oxygen masks, and flutter valves, should be properly cleaned and maintained to ensure that they don't harbour infectious organisms.
- Get vaccinated. Talk with your doctor about which vaccines you should get. In general, people with COPD should get a pneumococcal vaccine once, as well as a flu vaccine every year.
- Stay away from crowds. When possible, avoid large crowds, especially during cold and flu season.
- Treat infections as early as possible. Call your doctor at the first sign of infection, so it can be treated before it progresses to a more serious infection of your lungs.
- Breathe clean air if possible. Breathing in air from your supplemental oxygen unit and air that has been filtered in your home will be a lot cleaner and free from irritants such as pollen, dust and germs and will help to reduce the risk of an exacerbation.
References: www.webmd.com and www.buffalo.edu and http://lungdiseasnews.com and www.everydayhealth.com
COPD awareness: Nadia Sawalha experiences life as a COPD patient for a day
Many people would not volunteer to spend a day living their life in the shoes of a COPD patient, however TV presenter Nadia Sawalha did take on the challenge. She spent a day as a COPD patient with a very tight corset around her waist and a mask over her mouth in order to simulate the constrained breathing conditions of a COPD sufferer and having oxygen equipment to take around with her. She then tried to go about her normal daily activities such as shopping and cooking.
She found it difficult even doing the little things such as walking up stairs and manoeuvring around the kitchen. She found it difficult to reach up and down for things, constantly stopping to pause for breath or to hold onto a wall. She had great difficulty getting around as the wheezing and gasping for breath always seemed to get in the way.
“It's as if, when your airways narrow, so does your very life,” says Nadia. When asked about how she found the experience, she said that it was “truly horrific.” She recounts the feeling of “trying so hard to open your lungs” and being unable to have a conversation “because all you can think about is your next breath.”
Part of the reason that she undertook the challenge was because her nan suffered from COPD and she feels like she's become a bit closer to her nan as she understands a bit more now the daily challenges that she went through. It has also made her understand the challenges COPD patients go through everyday and that she is fortunate to still have normally functioning lungs. Being a former smoker, she is now a strong advocate of early COPD diagnosis, especially after knowing how it feels like to lose a percentage of your breathing capacity. She realises now why patients need to be on supplemental oxygen just to get around but also how having the equipment attached to you all day can infringe on your mobility. She encourages people to get checked immediately if they think they may have COPD, saying that “it is not something you always get tested for, so it’s good to ask your doctor.”
Even though there are many challenges to overcome, exercising and keeping active is one of the best things COPD patients can do, other than quitting smoking. Keeping active will pay off and prevent the disease from worsening quickly and improve your mental well-being and quality of life.
An understanding of COPD is much needed in today’s society, especially where we see patients walking around with portable oxygen equipment. Becoming more aware of this condition helps us be more considerate toward our involvement in producing pollutants like cigarette and exhaust smoke or in the use of chemical irritants like cleaning solutions.
At the end of the challenge when Nadia could remove the corset she breathed a huge sigh of relief and it made her realise how lucky she was. Though people with COPD cannot do the same and just take off any virtual corset to feel better, with the right treatment and proper daily habits, there is hope to feeling much better and being able to breathe more easily. Hopefully Nadia has helped raise awareness of COPD and the daily struggles that patients go through and hopefully will encourage people to stop smoking and polluting the atmosphere so that fewer people suffer in the future.
References: https://lovegoservice.wordpress.com