Regular exercise and help survival of COPD and asthma patients
COPD includes emphysema, chronic bronchitis and asthma and is often related to smoking. Common symptoms include difficulty breathing, chronic coughing, wheezing and phlegm production and over time can prove fatal.
Regular exercise could help boost the survival of people who've left the hospital after being admitted following an exacerbation. The risk of hospital readmission and death is especially high after a person has been hospitalized for COPD.
"We know that physical activity can have a positive benefit for people with COPD and these findings confirm that it may reduce the risk of dying following hospitalization," says Dr. Marilyn Moy from Harvard Medical School.
Having a difficulty to breathe often leads to a more sedentary and immobile lifestyle for patients and results in de-conditioning of multiple organ systems including the heart and muscles. It also results in a greater reliance on supplemental oxygen and medications and a general decrease in health. Improving muscle function with exercise has been demonstrated to decrease the chance of readmission to hospital. Exercise can avoid microscopic lung collapse and sedentary patients have a greater risk of developing blood clots.
Researchers in a Californian study found that those who did any amount of moderate to vigorous physical activity were nearly half less likely to die in the 12 months after hospitalisation than inactive patients. Even low levels of exercise reduced the risk by over 25%. The researchers believe that tracking physical activity levels might be a good way for doctors to pinpoint those COPD patients at high risk for death after hospitalization.
According to Dr Mensch, "COPD has now joined other chronic diseases, including type 2 diabetes and cardiovascular conditions, where exercise has been shown to decrease mortality and prolong life." This is particularly important for COPD as GPs have little to offer patients to help lower disease-linked death risk.
Another study in Australia has also shown that physical activity undertaken in small intervals spaced throughout the day can safely and markedly improve the health of people with COPD. The study established that 150 minutes of exercise per week is
most effective in reducing cardiovascular and metabolic disease, the development of cancer, and overall mortality.
Evidence shows that exercise can greatly improve the physical state and quality of life of COPD patients, reducing their breathlessness, and improving energy levels. Setting feasible exercise goals that incorporate physical activity into everyday tasks is a recommended option for COPD patients. The use of portable oxygen concentrators can help patients achieve these goals as these oxygen units allow the patients to move around with their oxygen supply whether indoors or outdoors and not be tethered to their oxygen tanks so they can move around, go for walks or exercise.
Researchers suggested that, in addition to trying to perform light exercises everyday, patients should focus on the reduction of sedentary behaviour, such as trying to spend less time sitting and taking short walks. Minor walks taken after sitting for a considerable time without breaks is highly recommended as for people with severe disease simple goals like this may be a more realistic place to start that trying to go for a 30 minute walk each day.
References: http://health.usnews.com and http://copdnewstoday.com
Science behind sighing
According to recent scientific findings, sighing—a universal expression of exhaustion, relief, or melancholy—is more than simply a reflex; it's an essential part of lung function.
Science behind sighing
Although sighing may appear to be just a deep breath, scientists have shown that certain brain cells are in charge of triggering this reflexive behaviour. A sigh is essentially two breaths taken quickly after each other, the second on top of the first. People usually sigh once every five minutes or so, and this seemingly insignificant action is actually very important for lung health.
Fact that sighing important
Sighing is mostly used to expand the alveoli, which are little air sacs in the lungs that are prone to collapsing. For the exchange of carbon dioxide and oxygen to be facilitated, these alveoli must stay open. Sighing adds twice the volume of air compared to a regular breath, so it effectively "pops" them open again. Lung failure would eventually result from collapsed alveoli that do not exhale.
Sighing is necessary for lung function, but too much of it can be harmful, especially when it's in reaction to psychological stressors like anxiety and despair. People suffering from respiratory disorders such as COPD may also find it difficult to exhale deeply, which can further impair their breathing. Comprehending the brain's function in controlling the rhythm of breathing and sighing is essential for creating focused interventions for those exhibiting irregularities.
Recent research has illuminated the complex mechanisms underlying this seemingly natural act by identifying certain brain areas and neurological networks involved in the production of sighs. Leading expert in this area Dr. Krasnow explains that the respiratory centre of the brain regulates not just the speed but also the kind of breathing, including coughs, yawns, sighs and more.
Better respiratory care
In the future, pharmaceutical therapies that target the processes that produce sighs may be possible. Further research is necessary to understand the underlying mechanics of conscious sighing and how it relates to emotional states.
The significance of using appropriate breathing strategies for those with respiratory disorders like COPD is highlighted by these findings. Good management includes both the inhalation and utilisation of oxygen, not only the addition of extra oxygen. The complex dance between the mind and body becomes more understandable as we dig deeper into the science of sighing, which eventually opens the door to better respiratory care and a higher standard of living.
References:
Iron could be the leading cause of COPD and its symptoms
Researchers have discovered that one in five people who suffer from chronic lung and respiratory conditions, such as COPD, have an iron deficiency. This may be causing worse symptoms for patients. About three million people in the UK have COPD and one dies every 20 minutes from the condition in England. People normally associate iron deficiency with anaemia but in fact iron is essential for many other processes in the human body and not just for making red blood cells.

Those with iron deficiency have much lower levels of oxygen in their blood, have greater difficulty exercising, require more supplemental oxygen therapy, suffer more frequent flare-ups and a worsening of shortness of breath, coughing and wheezing.
The Oxford study revealed a surprisingly big difference in oxygen levels between those patients with low iron and those with normal iron levels. “The amount of oxygen in the blood is a strong predictor of life expectancy in COPD, so these findings are potentially very significant for patients.”
Currently smoking cessation and treatments that target the air passages in the lungs are the main treatments for COPD patients. However some patients are still left with troubling symptoms that interfere with their daily lives and lead to hospital admission. Iron deficiency works in multiple ways to worsen the impact of COPD, hopefully establishing a new treatment regime with iron could improve things for these patients.
Excessive iron build-up in the lungs could be a major cause of COPD. A gene has been found to make certain individuals more susceptible to the lung disease. This gene regulates iron uptake in cells and is called IRP2. In mice those that lacked the gene remained healthy and those with the gene were symptomatic for COPD. A drug given to these mice however prevented additional lung damage and even reversed COPD's effects.
This study goes some way to prove that people may have a genetic predisposition to developing COPD. If this gene is expressed then there is an excessive build-up of iron in the cells, particularly in the mitochondria. Iron is needed by the cell but in a delicate balance and too much can cause haemochromatosis and leads to mitochondrial dysfunction and they cannot utilise oxygen effectively and cannot produce energy for the cell. This leads to inflammation and damage to the lung's air sacs and cells in the airways. When mice in the study were given a drug 'DFP' this drug binds to excess iron and relocates it to other cells in the body that actually need it and in doing so prevented and reversed the lung inflammation. This drug is already approved to treat thalassaemia and therefore could quickly be incorporated into a new treatment regime for COPD patients.
Therefore too much iron could be the cause of COPD and too little iron could worsen the symptoms. If further studies continue to prove these findings then it could not be too long before COPD could become a more treatable and reversible condition.
References: http://weill.cornell.edu and www.telegraph.co.uk
PARENTAL SMOKING WHEN YOU ARE YOUNG CAN INCREASE RISK OF COPD IN LATER LIFE
A new study has shown how people whose mothers smoked when they were young have a significantly increased risk of breathing problems and developing COPD later on life. The pulmonary disease consists of a group of lung disorders including chronic bronchitis and emphysema that harmfully affects airflow and breathing, to the point where the patient needs artificial oxygen supplement in order to breathe normally. The study was based on 50 years of follow-up on 8,000 youngsters and their parents which included lung function tests and questionnaires about their smoking habits.

There was no link between mothers who smoked less than 20 cigarettes a day, nor with whether the fathers smoked or not. However parents whose mothers smoked more than 20 cigarettes a day had nearly 3 times the risk of airflow obstruction in middle age compared to those who were not exposed as a child. Men seem more susceptible however and have nearly 4 times the risk of developing COPD compared to women who have 2 times the risk. Also interesting was that these figures are not impacted by the individual's smoking habits as they grew up.
It suggests that mothers smoking is linked to a reduced lung function in offspring when they get to middle-age and that a reduction in lung function in childhood may predispose to having a lesser lung function in adulthood.
The efficiency of oxygen transfer to the blood is also more significantly impaired in smokers who had mothers that smoked heavily.
It was already known that smoking when pregnant resulted in the baby having smaller lungs and that your maximum achieved lung function usually developed by 25 years is lower if parents smoked. The lungs continue to grow for a few years after birth, the number of alveoli increases and smoking exposure limits this growth. This study shows that in addition to affecting growth, parental smoking also leads to lung disease in later life for the offspring.
In addition second-hand smoke causes irritation and inflammation in the airways and chronic scarring of the airways makes them stiffer and smaller contributing to the development of COPD. Children who had parents who smoked are also more likely to be frequent smokers later on in adulthood, which also significantly increases the risk of lung damage and developing respiratory diseases like COPD.
It is becoming even more important that pregnant women and mothers do not smoke around their children as it harms their lungs from the start and predisposes them to a greater risk of lung disease in the future.
References: www.foxnews.com and www.pulseheadlines.com
Sleep apnoea can encourage cancer growth
A new study has shown how patients who suffer from sleep apnoea may leave themselves open to encouraging the growth of cancer tumours. The hypoxia caused by the condition results in blood vessel growth in tumours.
Sleep apnoea is a disorder whereby the patient has shallow breaths and pauses in breathing during sleep, which can last from a few seconds to a few minutes and can happen up to 30 times in an hour. This can be due to the airway becoming blocked or collapsing during sleep. Risk factors include a small upper airway, smoking, alcohol use, being overweight and having a large neck. Many patients who suffer respiratory disease also find that they suffer from sleep apnoea, especially COPD patients as a large proportion of COPD patients still continue to smoke.
Previous studies have linked sleep apnoea to an increase of death from cancer but this recent study has made the mechanisms a bit clearer. It seems that the intermittent hypoxia (reduction of oxygen in the blood available to the tissue cells) suffered by the patient during episodes of sleep apnoea encourages mechanisms that result in tumour growth. Mice that had tumours and experienced intermittent hypoxia (like with sleep apnoea) showed an increase in vascular progenitor cells and endothelial cells. These cells than can mature to create blood vessels in tumours. This increase in blood vessels within the tumour will allow the tumours to receive more oxygen and nutrients from the blood to encourage growth and for them to metastasise and spread throughout the body.
Also these mice showed an increase in levels of VEGF (vascular endothelial growth factor) which is a protein known to boost blood vessel formation. Overall the team behind the study believe that the findings indicate that sleep apnoea may worsen the outcome for cancer patients.
Dr. Vilaseca says "patients suffering from obstructive sleep apnoea usually suffer from intermittent hypoxia at night. This work shows that intermittent hypoxia has the potential to promote the formation of blood vessels within tumours, meaning that the tumours have access to more nutrients.”
Prof. Arnulf Stenzi comments that the findings are remarkable and shows how oxygen deficiency can really influence the body in many ways and especially in this case with tumours. "It may be postulated that increased oxygenation of the blood may be the underlying mechanism why not smoking or giving up smoking, regular sport activity, reducing the body mass index (BMI) and other lifestyle changes that increase tissue oxygenation have a supportive beneficial effect on better outcomes in….cell cancer.”
Further studies will be carried out as it opens up the question as to whether this only happens during sleep apnoea episodes or whether it could happen during the waking day with patients who suffer from shortness of breath with respiratory conditions such as asthma and COPD. It could make it even more vitally important that patients who suffer from conditions where blood oxygen levels drop ensure they are monitored and take their medication and supplemental oxygen regimentally both day and night to ensure that they are not risking an increase in tumour growth. Cancer can go undetected and you may not be aware that you have it but allowing your body to become hypoxic could be encouraging tumour growth; whether malignant or benign and worsening the condition and your outcome.
References: www.medicalnewstoday.com
Mesothelioma explained
Mesothelioma is a tumour of the mesothelium which is the thin lining that covers the outer surface of most of the organs in our body. More than 2,500 people in the UK are diagnosed with this disease each year.
There are different names depending upon where in the body it develops, for example in the chest it is called pleural mesothelioma and in the abdomen it is called peritoneal mesothelioma. The tumours can be malignant or just benign cysts. The main cause of mesothelioma is exposure to asbestos.
Asbestos is a natural mineral found in many countries and it acts as an insulator and was used to protect against fire and corrosion until it was banned in the 1980's. Mesothelioma doesn’t usually develop until many years after exposure to asbestos. It can take any time from 10–60 years, although the average is about 30–40 years after exposure. Construction workers, plumbers and electricians are more likely to have been exposed to asbestos and as these jobs were traditionally done by men, males are five times more likely to develop mesothelioma than females. Occasionally, mesothelioma develops in people who have never been exposed to asbestos. Mesothelioma has been linked to exposure to radiation and also to a mineral called erionite, which has been found in Turkey and North America. Mesothelioma isn’t infectious and can’t be passed on to other people. It isn’t caused by inherited faulty genes, so family members don’t have an increased risk of developing it, unless they have also been exposed to asbestos.
Pleural mesothelioma is more common and makes up 90% of cases. The pleura is the smooth outer lining that covers each lung. There are two layers of this lining; the inner and outer and they normally slide over each other as we breathe aided by a fluid that the layers produce. When mesothelioma develops here the layers become thickened and press inwards on the lung and sometimes excess fluid collects between the two layers which is known as a pleural effusion. It can sometimes spread to lymph nodes throughout the body. When asbestos is disturbed or damaged, it releases tiny fibres that can be breathed into the lungs and can make their way into the smallest airways of the lungs. The body’s defence mechanisms try to break them down and remove them but this leads to inflammation in the lung tissue. The asbestos fibres can also travel through the lung tissue to settle in the outer lining of the lung (the pleura). Over many years they can cause mesothelioma or other lung diseases to develop.
Symptoms include:
- shortness of breath
- heavy sweating (especially at night)
- fever
- chest pain that feels heavy and dull or aching
- weight loss
- loss of appetite
- a cough that doesn’t go away, although this is unusual.
Also a pleural effusion may cause shortness of breath and chest pain.
The peritoneum is the outer lining that covers the organs in the abdomen and helps protect the organs and keep them in position. It also consists of two layers; the inner and outer layers. Peritoneal mesothelioma causes a thickening of the peritoneum and sometimes excess fluid will collect and cause swelling of the abdomen, which is known as ascites. Asbestos fibres can be swallowed, and some of the fibres can stick in the digestive system. They can then move into the outer lining of the abdomen (the peritoneum). Here, they cause swelling and thickening of the lining and can lead to peritoneal mesothelioma.
Symptoms include:
- swelling in the tummy
- tummy pain
- loss of appetite
- weight loss
- feeling sick
- changes to your normal bowel pattern, such as constipation or diarrhoea.
Also ascites may cause swelling in the tummy, pain, sickness and loss of appetite.
Sometimes early symptoms of mesothelioma mirror those of other diseases or physical issues such as congestive heart failure, emphysema, weight gain, or constipation. These symptoms may include shortness of breath, constant chest pain or cough, night sweats, weight loss but fluid gain, bowel obstruction, swelling of the feet, and a build-up of fluid on a chest X-ray.
Treatment will depend upon the location and stage of the tumour but there are drugs, minor and major surgery, radiation, chemotherapy and supplemental oxygen that can help to relieve symptoms and fight the cancer.
A custom-made walker has been designed by mesothelioma specialist Dr. David Sugarbaker and is known as the 'Sugarbaker Walker'. It was designed to help patients recover quicker from surgery and to get them back on their feet and become more mobile. It includes everything that a patient needs; an oxygen tank, chest tube vacuum, IV pole, catheters and space for monitors. Its also on wheels with adjustable arm rests. It helps patients to be able to manoeuvre around with all their medical equipment and become mobile, resulting in improved and faster recovery from surgery.
References: www.macmillan.org.uk and www.mesotheliomasymptoms.com and www.asbestos.com/news
What is all the hype around meldonium?
Although medonium, also known as mildronate, has been produced lawfully in Latvia since the 1980s, the FDA has not given it approval for use in the US.
What is Medonium used for?
Being an "anti-ischemic" medication, it is used to treat organs—particularly the heart—that do not receive enough blood flow. It is mostly used to treat people with cardiac issues that interfere with the body's ability to absorb oxygen. It aids in preventing tissue damage from angina attacks, persistent heart failure, and circulation issues in the brain. It is also advantageous to healthy people and athletes because of its power to enhance oxygen intake, which improves mental clarity, physical endurance, and physical capacity. This is why it was banned by the anti-doping authorities at the beginning of the year and caught out a number of athletes who have tested positive, such as the tennis player Maria Sharapova.
How does it work?
Meldonium reduces the amount of oxygen that is needed to keep tissues alive by changing the way the muscle cells metabolise substances in the blood. It alters the mitochondria to utilise carbohydrates for energy instead of fatty acids, a process which requires less oxygen to carry out. Therefore in people with less oxygen in their blood they can still produce energy in the cells and the tissue and organs remain healthy. In athletes this reduction for the need of oxygen can enhance their performance. During exercise our bodies use oxygen at a faster rate than the lungs can replace it but this drug can reduce the amount of oxygen being used up allowing athletes to work out for longer. Processing carbohydrates instead of fatty acids also means that there is less lactate and urea produced, which would normally cause stiffness and pain in the muscles after a workout and so an athlete can workout out for longer and more frequently. Due to its ability to allow an athlete to work out more efficiently and for longer by altering the way the cells metabolize substances for energy, and diminishing the need for oxygen it has been considered as an unfair advantage over other athletes and has been banned.
There are other benefits
But the medication has more advantages, and when used with other medications, it can help cure diabetes by lowering blood glucose levels because it forces cells to metabolise carbohydrates, which include glucose molecules. Along with improving mood and motor abilities, it can help lessen dementia and improve cognitive function in people with neurological illnesses and circulation issues in the brain.
How can it support an oxygen user?
Patients with respiratory disorders like COPD may benefit from adding the medication to their therapy regimen. These individuals may have extremely low blood oxygen levels, for which they are receiving additional oxygen therapy in an attempt to treat it. As a result of the low oxygen, these patients may have extreme weakness and fatigue. By rerouting oxygen from the cells' energy metabolism to other areas where it is also required, medonium may enable the body to use less oxygen in the cells. Patients would benefit from having more oxygen in their blood and experiencing less weariness, both of which could slow the disease's course. Patients are urged to maintain their health and fitness and to engage in as much activity as they can.
Reference TechInsider
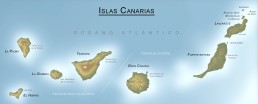
Your medical oxygen in Gran Canaria, Tenerife and other Canary islands
For nearly 22 years we have been arranging medical oxygen on the Spanish Canary Islands Not only Gran Canaria and Tenerife but also the smaller islands like La Palma de Gran Canaria, Hierro, Fuerteventura, Lanzarote and Gomera.

OxygenWorldwide provides Gran Canaria & Tenerife with LOX Liquid oxygen (LOX), concentrators (CON), portable concentrators (POC) and large cylinders (GOX /BOT).
For all other islands we can arrange concentrators (CON) and/or portable concentrators (POC) in combination with a stationary concentrator (CON) for use indoors and/or during the night.
OxygenWorldwide provides our own 'Airport Service' (A.S) in the 100 countries where we are active. We provide an Airport Service at all Canary Islands but in principal only during weekdays (Monday – Friday). But if you requires this service during the weekend please contact our 24/7 helpdesk (in 5 languages) to check whether we can still accomodate you and make this possible.
An Airport Servcie means that we have, on your arrival, someone at the door of the aircraft to hand you over a portable oxygen device so you can make your way to your hotel etc. with oxygen. On your departure we will again have someone at the door of the aircraft who will collect the equipment again from you. In case, due to custom regulations, we can not meet you at the door of the aircraft we will have someone to meet you in another place within the airport.
Mainly due to the perfect climate, especially in the winter time, many people spend their winters at one of the Canary Islands. As we at OxygenWorldwide have been in the medical oxygen business for over 22 years we know more than anyone else that being mobile is the most important thing when it comes to holiday making. Therefore we constantly strive to try to improve the provision of mobile oxygen equipment. For years only liquid oxygen was in demand and needed to be made to be mobile by means of a stroller, which was filled on a base unit. However currently many oxygen users prefer the portable concentrator.
In cases where you may want to bring your own portable oxygen concentrator but a back-up is required in case the POC might break down or is not suitable to use 24 hors per day, OxygenWorldwide can arrange a back-up cylinder for inhouse use and/or during the night.
For more info please contact OxygenWorldwide on info@oxygenworldwide.com or call us on +34 96 688 28 73
We hope you have a great stay on the Canary Islands.
OxygenWorldwide supplied medical oxygen to Dubai
As Dubai continues to emerge as a top holiday destination, OxygenWorldwide is proud to announce the on-going establishment of a local depot equipped with medical oxygen solutions. Since March 2016, we have been offering oxygen in compact aluminium cylinders as small as 2 litres, providing a convenient option for oxygen users seeking mobility during their stay.
To enquire about the availability of POCs or other oxygen equipment, please contact our 24/7 multilingual call centre at info@oxygenworldwide.com or call us at (+34) 96 688 28 73.
We provide larger alternatives, including 4.5, 9 and 45 litres, together with trolleys for increased convenience, in addition to small cylinders. Our goal is to guarantee that oxygen users have access to mobile equipment so they can take advantage of Dubai's stunning beaches and attractions, whether they are visiting the city as a destination or as a stopover.
OxygenWorldwide is dedicated to satisfying your needs with professionalism and knowledge, having served oxygen consumers globally since 1993.
Additionally, Airport Service (A.S.) is provided by OxygenWorldwide in more than 100 countries, including Dubai. When you arrive, our staff can give you a carry-on oxygen concentrator at the airport, making your trip to your hotel easier. To ensure a hassle-free travel experience, departing travellers can also return the equipment at the aeroplane door.
Please contact us for specialised arrangements and unique solutions in Dubai or other nations. Our goal is to ensure that your time in Dubai is worry-free and pleasurable. We appreciate your decision to work with OxygenWorldwide and hope you have an amazing trip to Dubai.
Your head can heal your body and even reduce oxygen therapy
Science is increasingly proving to us that what is going on in your brain can affect how the body heals, even from chronic conditions such as MS, chronic pain, HIV and COPD.
Obviously this should be used in conjunction with traditional treatments and medications, not instead of but science proves that what's in your head can speed up and improve your body's healing processes and it can influence everything from your immune system to pain control.

Our mental state has dramatic effects when it comes to the symptoms we experience like pain, fatigue, nausea and depression. Playing a virtual-reality game can ease pain in burn victims by 50% more than by drugs alone. Placebo painkillers trigger the release of natural pain-relieving chemicals called endorphins. Showing that our thoughts and expectations can have a similar effect that drugs do. If we feel stressed and alone then warning signs such as pain, fatigue and nausea are amplified and if we feel safe and cared for then our symptoms are eased. Ultimately are brain controls and creates the experience of any damage that has been caused to our body. Our mood and mental and emotional state plays a huge part in being able to amplify or ease symptoms. Studies have shown that patients receiving warm, friendly good quality care at the GP and hospitals showed an ease in their symptoms compared to those to had a more quick, abrupt, colder experience. So regardless of the treatment given, it can be how the care is delivered that can determine a patient's outcome and our recent trend of shortened 10min appointment slots and reduced staffing levels are in fact proven to be detrimental to patient care and outcome.
The brain controls physiological functions from digestion to the immune system and therefore is also relevant for the physical progression of the disease too. We cant wish ourselves better but by modulating our responses to stress we can influence our own brain into control our internal processes in a positive way to help reverse the progression of chronic conditions.
Stress of a situation can cause just as much harm as a physical injury for example in an earthquake just as many die from heart attacks as from falling rubble. Studies show that patients who feel negative or anxious before an invasive procedure will suffer more complications during and afterwards. Relaxation techniques have shown to vastly reduce pain and anxiety as well as the rate of adverse effects. Stressful situations can also effect our bowel movements and patients with IBS have found that gut-focused hypnotherapy teaches patients to tackle stress and calm their digestive system and is highly effective.
Stress also affects the immune system and in cases of long-term chronic conditions it can disrupt the healthy immune response and result in infections and auto-immune disease. It can accelerate MS and HIV conditions and recent studies have shown that stress-management therapy can stall progressions in MS and that mindfulness mediation can slow HIV.
There is also evidence that the mind plays a role in cancer. Stress hormones have been shown to make some cancers spread faster and an imbalance in the immune system can encourage the growth of tumours. Early results from studies show that stress-management reduces inflammation but we are still waiting to see if that translates into increased survival rates. Even if this isn't found to happen, easing the fatigue and nausea from chemotherapy may encourage someone to stick to their treatment plan and indirectly improve survival.
Patients with COPD have found that through relaxation, meditation and stress management therapy they can ease their symptoms and reduce the frequency and severity of exacerbations and reduce the amount of oxygen therapy they need.
The mind can't heal everything but it is clear that our mental state does have wide-ranging physiological effects that can affect our health in many ways even with those suffering chronic serious diseases. Trying to stay positive, feeling cared for and dealing with stressful situations can benefit your health.
References: http://www.thedailybeast.com