3 new treatments for COPD
COPD is a complex disease that is inter-linked with many other diseases and conditions with their own separate symptoms. In order to treat COPD successfully then a range of therapies and treatments is needed in order to combat the disease from all sides.
Recently scientists have discovered three new treatments for COPD patients. Using innovative approaches to help to improve lung function and curb patients' symptoms.
THE COIL:
The lungs can become over-inflated due to trapped air and surgeons have developed tiny coils that can be placed into the lungs to shrink them and restore elasticity. It showed an 18% improvement in lung function after implantation.
“When you release them into the lungs, they just coil up and what they do is they draw the hyper-inflated lung close together,” said Professor of Medicine, at The Cleveland Clinic.
Patients still usually require supplemental oxygen however the coils provide much needed relief and the patient can take deeper breaths and not rely on the oxygen as much.
THE FLUTE:
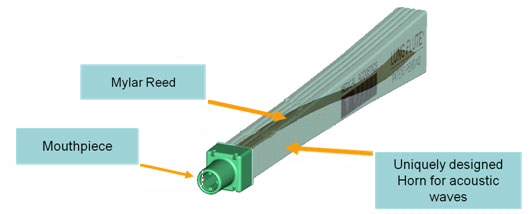
The second new COPD treatment is the Lung Flute, a medical device that improves lung congestion and clears mucus build-up if used twice a day, leading to higher quality of life among patients.
The Lung Flute technology produces low-frequency acoustic waves when the COPD patient blows into it. The acoustic waves are designed to reverberate into the lower airways to loosen secretions that are lodged deep in the lungs. The Lung Flute has been tested in clinical trials and is approved by FDA as a safe and effective form of treatment for COPD.
NEW DRUG:
There is also a new drug called azithromycin which is an antibiotic that has been found to considerably reduce the frequency and severity of flare-ups in COPD patients, if taken long-term, by 20%. The same approach of taking similar drugs long-term has also worked for other lung conditions such as cystic fibrosis. Rather than taking anti-inflammatories or antibiotics reactively after a bad spell, instead doctors use the drugs as preventative treatments and by taking them long-term they build-up and it helps to ease and reduce symptoms.
Depending upon your condition, its status and other medical conditions will mean that each COPD patients has a different set of symptoms and degree of severity and therefore by prioritising the worst symptoms and treating them with different approaches could greatly reduce many different symptoms and greatly improve their condition and quality of life. Ask your GP about different possible treatments and therapies and you may be able to get these products in the private market as they are more and more widely becoming available globally.
References: http://lungdiseasenews.com
WHAT'S THE BEST TREATMENT FOR SLEEP APNOEA?
For those suffering from respiratory diseases, sleep apnoea is often an accompanying condition. Sleep apnoea is a common and chronic condition in which breathing stops or becomes shallow during sleep. Breathing pauses can last from a few seconds to minutes and can occur 30 or more times an hour. Disrupted sleep and a reduction in the level of oxygen reaching the brain can increase blood pressure (leading to heart disease), reduce mental ability and leave you feeling tired and fatigued, in addition to your daily respiratory symptoms.
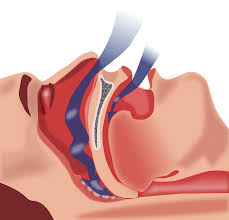
There are two common treatments for sleep apnoea; continuous positive airway pressure (CPAP) and mandibular advancement devices (MADs). A recent study has shown that both treatments not only are effective in reducing sleepiness and increasing oxygen levels while you sleep but also result in a lowering of both systolic and diastolic blood pressure rates.
MADs work by pushing the jaw and tongue forward to keep the airway open during sleep and are shaped similar to a gum shield. With CPAP the patient wears a mask connected to a device that produces mild air pressure and provides oxygen which helps to keep the airway open.
Some patients find it difficult to adapt to CPAP with problems wearing the face mask or being unable to sleep due to the noise of the compressor and find MADs a more suitable treatment but it does depend on what type of sleep apnoea you suffer from as to which treatment is more suitable.
In the study of 5000 patients both treatments were tested as to their effectiveness and ability to decrease blood pressure. There was no significant difference between CPAP and MADs in lowering blood pressure, they both were equally effective however CPAP was more likely to lower systolic blood pressure compared to MADs and would be slightly more effective in patients who are able to enjoy more hours of sleep.
Even though CPAP appears slightly more effective and are effective across the whole severity range, MADs are equally good as an alternative treatment for some patients who suffer mild to moderate sleep apnoea. The lowering of blood pressure achieved by the two treatments is modest so if you suffer from very high blood pressure you should get it checked regularly and take your medication to help to combat this.
Many patients find that by combating their sleep problems they feel much more able to face the day with their respiratory condition and in combination with oxygen therapy during the day or night they feel able to being able to carry out all their daily activities and feel near normal again.
References: http://www.webmd.com
THOSE WITH COPD MORE LIKELY TO SUFFER FALLS
A recent study has shown that if you suffer from a lung condition such as COPD then you are at a much higher risk to suffer from falls, especially if have other medical conditions, have already taken a tumble or have a long history of smoking.
Past research has already linked COPD to an increased risk of imbalance, muscle weakness, thinning bones and blackouts. COPD alone accounts for 5% deaths globally and falls are also a major public health problem, accounting for more unintended deaths and injuries each year than any other cause (except traffic accidents).
Most falls in the study occurred indoors, often when people were standing and using their upper body at the same time, with loss of balance the most commonly reported cause. It was found that people had more than twice the risk of falling if they suffered from additional medical problems and more than triple if they already had a fall in the previous year. The findings add to growing body of evidence highlighting the increased fall risk faced by COPD patients.
In another study it was also noted that those patients who used supplemental oxygen regularly were at a reduced risk of falls. This is probably due to the fact that oxygen levels are increased in the blood stream due to the use of supplemental oxygen and that the problems such as weakness and imbalance are reduced.
Just one fall especially in the more elderly of patients can result in anything from a bruise to a hip replacement and from an unnecessary trip to the GP or a long-term stay in hospital. Having an injury when you have difficulty breathing only adds to the severity of the injury and the recovery process and could hamper your progress and increase the severity of your condition and lessen your quality of life. COPD patients need to be aware of their increased risk of falling and injuring themselves and take precautions. If you are prescribed oxygen then ensure you use it as regularly as required and as prescribed. There are workouts designed to help improve balance and stability which can help to minimize the risk. Adjust your home and activities to reduce the likelihood of a fall; not using stairs as often, moving objects to lower heights etc.
References: http://www.reuters.co
A stomach bug may offer hope for COPD patients
New studies have found that patients with COPD have a 3 times higher risk of having a certain bacteria within them. The bacteria heliobacter pylori, which is usually linked to the development of stomach ulcers may also be the trigger for lung disease.
Smoking is the main cause of COPD but research suggests that a big role may be played by the bacteria. It mainly colonizes the stomach but evidence suggests that is accumulates in the ears, nose, skin and even the eyes. It has previously been thought to be only involved in stomach ulcers and stomach cancers but recent studies have shown that the bacteria is also linked to other cancers, glaucoma, gall bladder, auto immune disease, iron-deficiency anaemia and other conditions of the eyes, ears, nose and throat.
One theory is that COPD patients may have a high level of this bacteria due to childhood infections that affect lung growth and make them more vulnerable to disease. Early eradication of heliobacter pylori in childhood may enable full lung development and reduce the risk of COPD in later life. The discovery could open the way for new preventative strategies.
- pylori stimulates the release of cytokines, which have an inflammatory effect on the body. When the infection and bacteria are eradicated then cytokine levels return to normal and inflammation decreases.
The findings may point to new ways of tackling COPD, because H. pylori can be detected with a breath test and treated with antibiotics. So it could mean that a simple course of antibiotics could kill off this bacteria, reduce the inflammation and reduce the severity of COPD symptoms immensely or if caught early then prevent COPD from developing.
References: http://www.dailymail.co.uk
Iron deficiency can worsen COPD symptons
Scientists believe that those who suffer from lung disease may suffer more severe symptoms due to a shortage of iron, which could be easily rectified with regular intravenous iron injections.

Iron deficiency is more common in patients with COPD than in those without the lung condition, according to the results of a study published in the BMJ. Its been found that one in five COPD patients has iron deficiency and these patients also suffered from lower oxygen levels, more frequent flare-ups and increased shortness of breath and coughing. Iron-deficiency is traditionally associated automatically with anaemia but iron is essential for many other processes within the body.
“We were really quite surprised how big the differences in oxygen levels were between patients with low iron and those with normal iron levels. The amount of oxygen in the blood is a strong predictor of life expectancy in COPD, so these findings are potentially very significant for patients,” says Professor Peter Robbins from the University of Oxford who led the work.
Levels of C-Reactive Protein are significantly higher in iron-deficient COPD patients, which means inflammation. The inflammation is driving the iron deficiency and the idea that inflammation causes iron deficiency is important. It suggests that other conditions may also result in iron-deficiency caused by inflammation and that other conditions could be treated with iron to help reduce the secondary symptoms caused by a lack of iron. Intravenous iron therapy has been shown to be beneficial in other chronic disease and should be explored as a potential new treatment for COPD patients.
Giving up smoking is the most important thing to do if you have COPD but many patients are still left with troubling symptoms that interfere with their daily lives and can lead to hospital admission. The current treatments target the airways which helps some symptoms but doesn't improve the patient's exercise ability and quality of life as much. Iron deficiency seems to act in a variety of ways to worsen the impact of COPD so treating patients with iron can help improve patient's quality of life, exercise abilities and general symptoms and reduce exacerbations.
There is the counter argument that iron injections would not resolve the problem as the patients usually are not short of iron in their food intake, it is just how the body utilises the iron when suffering from bouts of inflammation that causes the anaemia. Increasing the levels of dietary iron intake will therefore not resolve the issue however perhaps taking iron in the form of a supplemental multivitamin may help.
More research is needed into how best to correct the iron-deficiency and improve the lives of COPD patients.
References: http://www.telegraph.co.uk and http://www.pharmaceutical-journal.com
10 Christmas gift ideas for someone with COPD
Obviously friends or family with COPD do not just want presents all about their illness but if they have been newly diagnosed or need items replacing then you might be able to get them the perfect present. Anything that can help them with their disease will mean that you've helped to improve their quality of life all year round.

- Exercise Bike
Nothing is more important to the person who has COPD than exercise. Exercise helps build endurance and muscle strength, ultimately making it easier for your loved one to breathe. An exercise bike helps that person to enjoy exercise within the comfort of home with their oxygen nearby for peace of mind, and they can use it all year round in any weather condition, unlike a normal bike.
- Pulse Oximetry Monitor
An FDA approved pulse oximetry monitor allows the patient to monitor their oxygen levels to ensure that they are getting enough.
- Automatic Blood Pressure Monitor
Many patients suffer from COPD complications and may take a variety of different medications for them. A blood pressure monitor is essential to make sure the medications or the condition are not affecting their health.
- Nebulizer
A nebulizer is important to have as it administers medication directly into the COPD patient's airways to help them to breathe easier. Handy to have one when out and about so that if an attack happens they can try to reduce it and improve their breathing as a short-term tactic until they can get to their oxygen supply.
- Knitted Beret, Scarf and Gloves
Keeping warm is so very important for someone with COPD as cold air can trigger an attack and they will help to prevent them from catching any bugs during the winter.
- Nebulizer Carry Bag
This will allow them to take their nebulizer out and about with them more easily and help to encourage them to keep themselves active. It could be used to carry other small pieces of equipment too.
7.Extended Oxygen Tubing
If they feel slightly shackled to their oxygen tank then getting them some extended tubing will allow them more freedom of movement in their home to be able to do more homely activities and keep them more active at home.
- COPD for Dummies Book
A great beginner's guide for someone newly diagnosed or their partner or carer with lots of tips and advice on how best to cope with COPD. Also if they are smokers then perhaps self-help books on stopping smoking could also be beneficial.
- Portable Concentrator
If their local provider cant provide them with one then you can buy one privately. A portable concentrator is a hugely beneficial piece of equipment as it allows the patient to leave their home free from the shackles of their tank and use oxygen easily outside. It gives the patient a huge new lease of life and allows them to exercise, go shopping, see friends etc. without having to take their oxygen tank and supporting equipment with them.
- Accessories
There are lots of accessories available to help improve the home for patients who use oxygen. Sometimes local providers have limited choice and availability of these neat gadgets but private companies have a vast choice of those small things that can make a huge difference.
References: www.copd.about.com
Lung freezing may be a new treatment for COPD
Bronchitis is one of the diseases that falls under the COPD umbrella. It is where the main airways become inflamed and irritated leading to shortness of breath, mucus build-up and severe coughing. The new treatment being tested on patients with chronic bronchitis targets the thickened airway tissue by freezing it via a technique known as cryotherapy.
The theory behind it is that the cycle of freezing and thawing destroys the damaged tissue in the lungs allowing healthy cells to develop in its place and helps to repair the lungs and improve breathing. This has already been used to successfully treat oesophageal cancer.
A catheter is inserted into the airway and navigated to where the airways are thickened via an MRI scan and then liquid nitrogen at -200C is sprayed onto that section. The section of lung tissue is then allowed to naturally thaw for a few minutes and then the area is repeatedly blasted until the target tissue has been destroyed. The flash-freeze and slow thaw of the tissue has been shown to destroy the targeted cells but does not affect the collagen, which provides the scaffold for healthy tissue to regrow into.
This is currently being trialled in several British Hospitals and appears to be successful. The treatment can be adapted according top the patients needs and the number of treatments will depend upon the severity of their condition and how much tissue needs to be frozen. Hopefully these trials are the start of a journey towards a new successful treatment for COPD.
The medical potential is vast as it could mean that damaged tissue anywhere in the body could be treated by cryotherapy in the same way and allow new tissue growth to come through, thereby allowing aided self-healing of a huge number of conditions.
References: www.dailymail.co.uk
SLEEP APNOEA MAY CAUSE ALZHEIMER'S AND SUPPLEMENTAL OXYGEN COULD PREVENT IT
Alzheimer's disease is the most common form of dementia, which is a set of symptoms that include memory loss and problems with thinking, problem-solving and language. It is a physical disease that affects the brain and proteins build up in the brain forming 'plaques' and 'tangles' around the nerves. Connection is then lost between the nerves cells and leads to the death of the nerve cells and loss of brain tissue. Patients with Alzheimers also have a shortage of important chemicals that help to transmit signals around the brain. The disease is progressive and as more of the nerve cells die and brain tissue is lost, the more severe the symptoms.
Sleep apnoea is a condition where the walls of the throat relax and narrow during sleep and interrupts normal breathing patterns. During an episode the lack of oxygen triggers your brain to pull you out of your deep sleep so that your airway reopens and you can breathe normally. After falling back into a deep sleep again further episodes can occur even as frequently as every few minutes. Most patients snore loudly and have laboured and noisy breathing and is often interrupted by gasping and snorting. This repeated sleep interruption can make patients feel extremely tired during the day and suffer from reduced mental ability. However unless a partner or family member notices your symptoms whilst you sleep you may not know that you suffer from this condition and many people go undiagnosed.
Recent studies have shown that sleep apnoea may quicken memory decline and bring forward the onset of memory impairment conditions like Alzheimers by 10 years. The development and progression of Alzheimers may also be speeded up by sleep apnoea as well. These studies also revealed however that sleep apnoea patients that were being treated with supplemental oxygen overnight delayed the onset of memory impairment problems by as much as 10 years. Patients with sleep apnoea who were being treated declined at the same rate as volunteers who did not have sleep apnoea showing that being treated by oxygen counteracted the harm being done by the condition. It appears that the frequent drops in oxygen levels during episodes of untreated sleep apnoea have a major impact upon memory impairment and can directly lead to the early development of Alzheimer's and dementia. Also during sleep is when the brain has time to remove harmful waste products, if sleep is disturbed then there is an accumulation of harmful proteins that block nerve cell function. Certain parts of the brain are more sensitive to drops in oxygen levels than others; certain neurons in the hippocampus (where Alzheimer's is thought to start) is especially sensitive to drops in oxygen and sleep apnoea may 'stress' these neurons out.
There are currently no medications that can prevent the progression of mild cognitive impairment to Alzheimer's disease or dementia so treating at-risk patients with CPAP (oxygen treatment for sleep apnoea) is a prevention method that is worth trialling and testing. Previous research has already shown that CPAP treatment and supplemental oxygen at night slows and improves cognitive impairment in patients with Alzheimer's disease and increases brain tissue and now this more recent research backs up these findings. Hopefully soon there will be trials to prove whether supplemental oxygen at night could be the next new treatment for Alzheimer's and dementia patients or even those who are at risk.
References: www.nbcnews.com, www.alzforum.org, www.alzheimers.org.uk and www.nhs.uk
What is PAM?
PAM stands for pulmonary alveolar microlithiasis, which is a rare lung disease. It is where small stones accumulate in the alveolar air sacs in the lungs and therefore makes it increasingly difficult to breathe. The cause has been found to be due to a DNA mutation which results in the loss of a cellular pump which would normally remove excess phosphate from the air sacs. As a result there is a build-up of calcium and phosphate which leads to the formation of microliths or stones. These cause chronic inflammation, lung tissue damage and scarring and respiratory failure and patients require a continuous oxygen supply of a high oxygen concentration in order for patients to be able to get enough oxygen into their bodies to function.
New research has identified biomarkers, which may hold the key to being able to treat this rare and debilitating disease. It seems that the condition causes elevations of certain proteins (cytokines and surfactant) in the blood. By monitoring these levels doctors will be able to follow disease progression and treatment response in patients.
Another finding was that the stones dissolve in EDTA which is used currently as a treatment for heavy metal poisoning. If the lungs can be washed in a solution containing EDTA then the stones could be dissolved and reduce the burden being placed on the air spaces and relieve respiratory symptoms. As long as there are no toxic side-effects then this could become a new therapy for patients with PAM.
As the stones are caused by excess phosphate it has been surmised that a low phosphate diet may be able to prevent the formation of the stones, however a phosphate-restricted diet brings with it other medical problems such as rickets. Another possible idea is to restore the function of the pump in the cells by inserting a phosphate pump gene into the DNA of the cells using viral vectors.
"This study demonstrates how discovering the causes of these rare lung diseases not only can inform us how the lung normally functions, but can also lead us to potential therapeutic interventions for these rare and often lethal lung diseases,” says James Kiley, PhD, Director of the Division of Lung Diseases at NHLBI.
Rare disease research can reveal insights into the fundamental biology of the lung and this study for PAM has revealed a potential role for phosphate in the regulation of surfactant balance in the lung and have attracted the interest of cystic fibrosis scientists who may be able to use the findings to help treat CF.
References: http://healthnews.uc.edu and http://medicalxpress.com
PINEAPPLE JUICE COULD HELP WITH YOUR COUGH
Pineapple juice has been shown to be 5 times more effective than cough syrup. It fights infection, kills bacteria, loosens mucus and suppresses coughs.
 Pineapple juice contains an enzyme called bromelain, which has anti-inflammatory properties and is effective to combat lung inflammation. It is used to treat arthritis and is also used in the treatment of inflammation and swelling in the nose and sinuses. 1 cup also contains half of your daily requirement of Vitamin C intake. Vitamin C is essential because as well as many other uses, it also enables your body to metabolize certain vital enzymes that regulate your metabolism and manage energy. Pineapple juice also contains manganese, which is a mineral that helps form healthy connective tissue and bones. It also works to absorb more calcium, metabolize carbohydrates and fats and increases regular nerve function. Pineapple juice helps to soothe sore throats and helps to loosen and expel mucus from your lungs more easily.
Pineapple juice contains an enzyme called bromelain, which has anti-inflammatory properties and is effective to combat lung inflammation. It is used to treat arthritis and is also used in the treatment of inflammation and swelling in the nose and sinuses. 1 cup also contains half of your daily requirement of Vitamin C intake. Vitamin C is essential because as well as many other uses, it also enables your body to metabolize certain vital enzymes that regulate your metabolism and manage energy. Pineapple juice also contains manganese, which is a mineral that helps form healthy connective tissue and bones. It also works to absorb more calcium, metabolize carbohydrates and fats and increases regular nerve function. Pineapple juice helps to soothe sore throats and helps to loosen and expel mucus from your lungs more easily.
The study also indicates that the bromelain naturally present in pineapple may provide similar effects if the cough you suffer from is due to asthma. Pineapple juice has also been used to treat other respiratory ailments such as bronchitis, hay fever, asthma and pneumonia. It’s even being tested as a possible treatment for cancer and HIV.
Drinking pineapple juice instead of cough syrup is less expensive and has no toxic chemicals. Also a study also showed that when using pineapple juice patients recovered nearly 5 times faster from their ailments and exhibited a decrease in other symptoms related to coughing such as hacking.
If you suffer from persistent coughing from respiratory conditions such as COPD and asthma then by drinking pineapple juice not only does it soothe related ailments from persistent coughing but it suppresses the cough and helps to loosen mucus build-up and also aids in combating lung inflammation. This in itself can hugely improve your quality of life, help you to breathe better and help to reduce your symptoms and improve your condition. The naturally-occuring components also have other health benefits to aid in your overall health.
References: http://preventdisease.com and http://www.survivalmagazine.org










