Lung Conditions Shouldn't Stop You From Planning A Holiday This Summer!
There is a myth that if you are on oxygen therapy then your life is effectively over and that it is too restrictive and complicated to go away on holiday. This is not necessarily the case and for most sufferers the world is your oyster. Always check with your doctor first to ensure you are fit enough to travel and ask your doctor to write a letter stating this just in case you need it.
All you need to do is prepare and plan the holiday well and ensure that you consider some factors when planning your trip:
• Climate: many people with lung conditions prefer warm climates that have salty air. Lower oxygen levels at higher altitudes can make breathing difficulties worse.
• Terrain: whether your destination is flat or on a hill could affect your ability to get around comfortably.
• Wheelchair access.
• Transport availability.
• Special needs such as oxygen treatment.
• Plan in advance: if you leave things to the last minute, you could forget something crucial. Think about how far you can walk, how many stairs you can manage, access to toilets and what transport you can use.
• Be realistic: places you liked in the past may not be suitable now. Pick something you and your carer can cope with physically.
• Shop around: different companies have different policies for people with lung conditions, so find the best deal for you. Many travel agents offer holidays for people with special requirements.
• Ask questions: travel firms are used to dealing with special requirements. They should be able to answer all of your queries and concerns.
Arrange Insurance
You should ensure that you and your carer have full travel insurance before going away to avoid huge medical bills if you are taken ill during your trip. Look into this first as it may be expensive and you may need a specialist provider depending on your health. Check that it covers all aspects of your medical condition and that you declare everything accurately to them otherwise it may not be valid, leaving you with a huge bill.
Keep your documents safe with you while you travel in case you need them suddenly in an emergency.
The European Health Insurance Card (EHIC) entitles you to reduced cost – sometimes free – medical treatment if you fall ill when travelling in Europe.
Choosing Accommodation
Accommodation in the UK is divided into four mobility categories:
• Category One – suitable for people able to climb a flight of stairs that have extra fittings to aid balance.
• Category Two – suitable for someone who needs a wheelchair some of the time but can manage a maximum of three steps.
• Category Three – suitable for people who depend on a wheelchair but who can transfer unaided to and from the wheelchair in a seated position.
• Category Four – suitable for a person who depends on the use of a wheelchair and needs help from a carer or a mechanical hoist to transfer to and from the wheelchair.
Each category has its own logo, which is displayed by accommodation providers that have been assessed. Make sure you choose accommodation that best fits of requirements.
Other countries have different systems so just make sure you ask your travel agent about how to choose your accommodation abroad.
Getting There
Coach
Several coach companies are working towards making their vehicles accessible for people with disabilities. Many coaches now feature kneeling suspension, which makes boarding and alighting easier. Most on-board toilet facilities are now level with the coach seating.
Some companies allow you to bring on board your own oxygen supply and will carry some types of collapsible battery-powered wheelchairs.
Train
Different train companies have different policies regarding people with disabilities, so plan your route in advance and find out which companies’ trains you need.
Ferry
Many ferry companies have lifts, toilets and wheelchair facilities; some can supply wheelchairs at terminals. A few have special cabins for disabled people and/or offer discounts. Check before you book, especially if you need oxygen.
Camping and caravanning
The Camping and Caravanning Club has three stages of accessibility for camping and caravan sites. So you just need to check that the site is appropriate for your needs.
• No accessible facilities;
• Accessible to people who can move around a little, but not wheelchair accessible; and
• Fully accessible including shower blocks and facilities.
Holidaying With Oxygen
Oxygen for travel in the UK is provided by the NHS. You just need to let your usual oxygen provider know the details of your holiday, including the dates you are going and returning and where you will be staying, and they will arrange everything for you.
You should first get permission to store oxygen cylinders and equipment from the owner of the place where you are staying.
Oxygen suppliers in the UK will only provide oxygen for travel and stays within the UK. If you are travelling abroad then there are many overseas oxygen providers that can fulfil your oxygen requirements and if you are travelling by plane then you need to ensure your airline's oxygen policy and whether you need to complete any additional documentation for them.
Flying with a lung condition
Many people believe their lung condition will prevent them from flying, especially if they need oxygen but this is not necessarily true. First, ask your doctor whether you can travel by plane and whether you will need any additional oxygen on the plane.
Then contact individual airlines to discuss your requirements and to find out what their policy is for carrying and using oxygen on planes.
If you are planning a long-haul flight and use a continuous positive airway pressure (CPAP) machine to treat the sleep disorder obstructive sleep apnoea (OSA), you should consider whether you might need to use your machine during the flight.
Some airlines have restrictions on what machines are permitted for use on board and others may require you to fill in a form before you travel.
When you contact the airline, find out what assistance is available at the airport as well as on the plane and check:
• the airline’s policy on carrying and using oxygen and medical devices such as CPAP machines;
• the exact length of the flight, and whether delays are likely;
• the facilities available at the outgoing and incoming airports. These might include assistance to get you from the airport lounge to the departure gate and on to the plane, the use of wheelchairs, and whether oxygen is available at the airport; and
• how you should confirm your fitness to fly.
Medication
If you are on medication then you will need a letter from your doctor confirming that you need the medication, and you should also keep a list of all the medication and doses you take in case you need to get more during your stay. List the proper names, keep all medication in its original packaging and keep it with you in your hand luggage. A doctor’s letter is required for liquid medicines exceeding 100 millilitres that are taken into the aircraft cabin. When given medication abroad, check whether it can be brought back into the UK. If you are in any doubt, declare the medication at customs.
Preparation is the key. Plan your trip in advance, think through everything you need, ask as many questions as you can of as many people as possible, then decide what’s best for you.
References: http://www.blf.org.uk and http://www.cancerresearchuk.org
Extreme Weather Can Trigger Your Asthma

For most people, if their asthma is managed properly and under control then the weather should not have much of an effect, however for others extreme weather conditions can bring on symptoms and organisations suggest extra thought and care is taken before heading out in it.
Changes in temperature of the air within your airways can cause inflammation, for most this is not a problem as the nose controls humidity and temperature. With people who suffer from asthma, they tend to breathe more through the mouth and irritants, pollutants and pollen are more of a factor and many already have inflammed airways. The more severe the asthma, the more likely it is that the weather will affect them.
Common weather triggers include:
• Cold air can cause constriction of airways.
• Wind and rain-Rainfall can increase and stir up mould spores, and wind can blow around pollen and mould.
• Heat-increased ozone from smog, exhaust fumes, and pollutants tend to be higher. Dry hot air can also trigger asthma.
• Lightning-Thunderstorms, which can generate ozone, are now thought of as an asthma trigger.
• Air pressure fluctuations-Barometric pressure can trigger sinus episodes and sinusitis is a common asthma trigger.
Cold Winter Air:
75% of asthma sufferers say that cold air can trigger asthmatic symptoms. The advice is to ensure that you are managing your asthma and taking any prescribed medication. Just as important is to be prepared. Check the forecast and make sure you carry your inhaler with you, wrap up warm and dry and wrap a scarf around your nose and mouth and try breathing more through your nose and it will help to dehumidify and warm the air up.
Remember that the difference between inside and outside temperature can be a factor so even going in and out of heated shops, or going from a nightclub or pub out into the cold air are all times when you need to look after yourself.
Exercise is very beneficial for people with asthma as it can help improve lung function and improve fitness but over three quarters of people with asthma have told Asthma UK that exercise in colder weather is a trigger for their condition. This is mainly due to the fact that during aerobic exercise you would inhale more of the cold air, breathing it in through your mouth (which means that it is not warmed or moistened by your nose) and breathe it more deeply into your lungs.
There are many things you can do to maintain your exercise regime but avoid the triggers.
• Exercising indoors or at a gym or gym classes instead of venturing outside.
• Warm up and warm down for 10-15 mins before and after outside exercise.
• Dress appropriately with a scarf around your throat and nose.
• If symptoms begin stop exercising immediately, take your inhaler and wait until you feel better before you resume.
• Consider more moderate exercise that will reduce the need for such deep breaths like a power walk instead of a run or a more gentle bike ride.
When it is cold many avoid going outside to try and avoid the triggers, however spending more time indoors exposes you to more triggers within the home such as pet hair, smoke, dust mites, fireplaces etc. Many sufferers prepare themselves for this and from being out in the cold by having a back-up home oxygen supply to use when the cold weather has triggered off a bad asthma attack.
Thunderstorms:
More recently it has become apparent that thunderstorms can trigger serious asthma attacks, especially children and young adults, with large numbers of people needing to go to A&E.
It is not fully understood why this happens, but it is thought during a thunderstorm, the windy conditions cause high levels of pollen and mould spores to be swept up high into the air where the moisture breaks them into much smaller pieces. As the pollen and mould particles then settle back down, these smaller pieces of pollen and mould can be breathed into the smaller airways of the lungs where they irritate the airway and trigger asthma symptoms.
Not all thunderstorms trigger asthma, it seems to depend upon the time of year, the humidity, wind, air pressure and whether ozone levels are high.
The advice is to be aware of weather forecasts, try to avoid being caught outside in them and make sure you carry your inhaler.
References: http://www.everydayhealth.com/asthma and http://www.asthma.org.uk
The Truth About Oxygen Bars: Healthy Trend or Just Hype?
You may not believe this but customers pay to breathe in 40% oxygen through a plastic hose that is placed into their nostrils at oxygen bars, which first appeared in the US in the late 1990s. You may also select from a variety of oxygen flavours, like peppermint, cranberry, or even scented candles. The length of the oxygen experience varies based on the customer's budget and preferences, usually lasting between a few minutes and roughly twenty minutes.
What Are The Promises of Oxygen Bars?
Although the proprietors of oxygen bars take care not to make any medical claims, they advertise their services for leisure and rely on client endorsements. Benefits like less stress, relief from pollution, more energy and alertness, better hangover recovery and relief from headaches and sinus issues are among the many advantages that users frequently mention.
The Science of Oxygen Bars: Is It Real or Is It Hype?
Despite these assertions, there are no extensive, carefully conducted scientific studies that back up any advantages of oxygen inhalation for healthy people. According to the American Lung Association, breathing oxygen is unlikely to have any physiological advantages for healthy individuals. Conversely, there's no proof that breathing in oxygen is hazardous either.
Oxygen Bars and Health Issues
Oxygen is usually given at home under a physician's supervision to patients with illnesses that impair lung function. Medical experts advise against giving these individuals oxygen bars because each person has different oxygen needs that need to be checked and adjusted by a healthcare practitioner. Uncontrolled oxygen use may be harmful, possibly resulting in dangerous oxygen intake levels or interfering with continuing medical care.
Fears Relating to Flavoured Oxygen
The usage of flavoured oxygen is one of the main issues with oxygen bars. These flavours are produced by pushing the vaporised aroma through the hose after bubbling oxygen through bottles containing aromatic solutions. While some bars employ food-grade, oil-free particles to create the scent, others might use aroma oils. Lipoid pneumonia is a dangerous lung inflammation that can be brought on by breathing in greasy materials. The purity or sterility of the fragrances cannot be ensured, even with oil-free mediums, which presents a risk for bacteria, allergies, irritants, and other pathogens.
Furthermore, a lot of oxygen bars can be found in places where smoking is allowed, such as casinos and nightclubs. Because oxygen can fuel combustion and increase the risk of fires, this poses safety issues.
Regulation and Research Are Necessary
Before oxygen bars are considered safe for use by healthy individuals, more thorough testing, research, regulation and medical oversight are required. It is now deemed dangerous to change a patient's course of treatment for medical disorders that call for oxygen therapy. Scientific research may someday corroborate testimonies, but for the time being, the claimed advantages of oxygen bars are mostly unsubstantiated and may even be psychological.
See MedicineNet and WebMD for additional details.
Oxygen Therapy and Autism
Hyperbaric Oxygen Therapy (HBOT) has only recently in the last two years been used to treat children with autism but with amazing results.

A study in 2012 by DA Rossignol et al proved that children with autism who received hyperbaric treatment for 40 hourly sessions showed significant improvements in overall function, receptive language, social interaction, eye contact, and sensory/cognitive awareness compared to children who received just pressurized room air.
When a person concentrates on a task or to generate speech, the brain is doing more work and there is an increase in blood flow to the brain, specifically the parietal frontal cortex, which is located behind the forehead. This increase in blood flow supplies the brain with more oxygen and glucose, giving the cells their needed energy to perform their task. In autistic children the opposite happens, they have diminished blood flow to begin with, and when their brain is attempting to perform a task their blood flow does not increase and does not supply the brain with the necessary oxygen and glucose the cells need.
The theory behind using HBOT on children with autism is that the increase in oxygen will reduce excess swelling of brain tissue, increase cerebral blood flow and stimulate cerebral tissue. There are correlations linking it to being able to remove toxins, reduce inflammation allowing oxygen deprived areas to have a return of blood flow, builds new capillaries in the brain and reduces the inflammation in the gut.
The belief is that all of these results will allow the brain to do its job better, resulting in a child who is more "present" in regards to social interaction and communication.
Studies and parents have reported that autistic children showed improvement in sleep, children becoming calmer and more affectionate, improved focus and attention, improved bowel function, improved cognitive and linguistic skills, being less sensitive to noise and appearing more 'present' and 'connected' to family members.
There are some unknowns however, such as any long-term affects, whether the treatments are long-lasting or not and whether certain autistic sufferers respond better than others. HBOT is definitely not a cure but it appears to be able to help some autistic children improve their behaviour, cognitive functions and quality of life and bring them a step closer towards 'normal'.
References: http://freshstarthyperbaric.com/adhd.php and http://oxfordhbot.com/hbot-for-autism/
Could Oxygen Make You Smarter?!
Research carried out at the Human Cognitive Neuroscience unit at the University of Northumbria, have discovered that mental performance can be greatly improved by inhaling a shot of oxygen.
Our brains only account for 2% of our body weight however it consumes the most energy (20-30%) out of all the organs but yet it cannot store very much energy and relies on a constant supply via the bloodstream.
In the tests students were given a one-minute blast of oxygen after being asked to remember a list of words. They remembered more words than those who didn't take any additional oxygen. Other students took oxygen whilst they were playing the higher levels of Tetrix, a computer game and it was found that they performed much better compared to students who didn't take any additional oxygen.
It would appear that additional oxygen blasts can aid in the brain performing at an increased level while it is attempting more demanding tasks.
Dr Sholey adds; "Even the most esoteric brain functions obey biological rules. By tweaking fuel availability to the brain, simply by throwing a bit more fuel on to the fire, you can improve cognitive function to some degree."
Cognitive improvement has been recorded in patients who use oxygen therapy at home but can also be linked to the research that has been carried out that suggests exercise will make you smarter. Exercise will improve your cardiovascular system which will in turn increase the amount of oxygen being pumper round the body. The brain relies on the bloodstream for it's oxygen supply and therefore will receive the optimal amount of oxygen possible if we are at our fittest. More fuel means more energy, which results in improved brain function.
However there is also research and studies that suggest that short periods of hypoxia (oxygen deficiency) also aids in increasing and improving oxygenation levels in the body and brain and could also aid in improving brain function ability. It is thought to be the reason why so many people who live in mountainous regions (where due to the altitude the oxygen levels in the air are a lot lower) live a lot longer. It is thought that a temporary, brief state of hypoxia causes reserve capillaries to open up, increase the amount of erythrocytes in the blood, increase the amount of circulating blood and increase blood supply to tissues. It is believed to improve your mood, immunity and metabolism as well as mental and physical capabilities. The idea was tested via a mask that alternated between a gaseous mixture containing normal oxygen levels and one that contained a much lower level. A similar affect can be carried out by ourselves easily by adjusting our breathing patterns and letting out a very long exhale, which will create a temporary hypoxic state.
References: http://www.theguardian.com and http://www.intellectbreathing.com
Let's talk liquid oxygen...
When oxygen is in a cold state ( -183ºC), it turns to liquid. More oxygen molecules fit into the same space when in liquid form compared to when it is a gas and so liquid gas only takes up 10% of the space that compressed oxygen does. Therefore this liquid allows for a greater amount of oxygen to be placed in a tank and it weighs less than a compressed oxygen tank.
Liquid oxygen is stored in an insulated stainless steel low pressure container that works in a similar way to a Thermos flask. These base units store and hold the liquid oxygen at an extremely low temperature. As with the compressed oxygen, it can be filled into smaller units from the base unit so that it can be used portably.
Liquid oxygen doesn't require power via electricity like oxygen concentrators do and also they make no noise.
There are some disadvantages in that liquid oxygen is more expensive than compressed oxygen and does not have as long of a shelf life as it will evaporate over time. Also, you will not be able to take liquid oxygen on a plane.
References: http://www.uk.airliquide.com and http://www.inogen.com
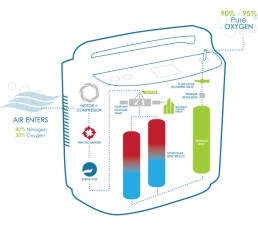
How Portable Oxygen Concentrators Work
The air around you contains about 80 percent nitrogen and 20 percent oxygen. If you require the use of portable oxygen to aid with a medical problem then you require a much higher percentage level of oxygen which can be delivered straight to your lungs by portable/at home devices. One such device is an oxygen concentrator.
How They Work:
Your oxygen concentrator takes in air from the surroundings and splits the oxygen from the nitrogen. It then releases the nitrogen back into the surrounding air. The concentrator collects and stores the oxygen and then dispenses it back to the patient.
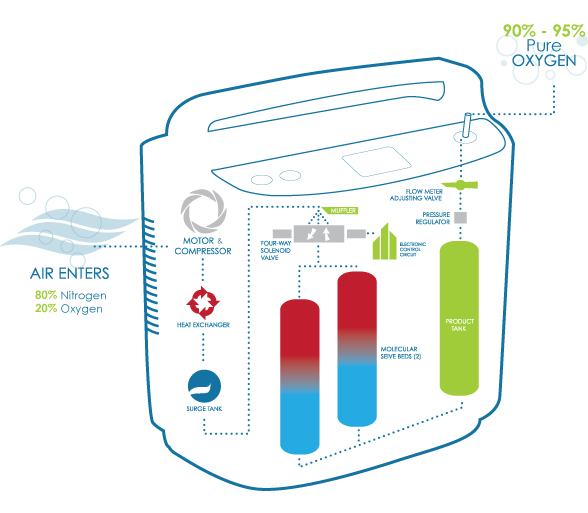
As long as you have it running and set properly, your oxygen concentrator is continually "making" 90 - 95 percent pure oxygen out of normal air, so you'll have all you need.
Oxygen tanks are already pre-filled with oxygen and have to be re-filled whereas concentrators can make oxygen as it goes. Tanks also run the risk of leakage, which can cause explosions/fires and are heavier and more difficult to move around with.
Concentrators do not pose any danger and the other main benefit is mobility. Most of the concentrators are portable, which means they're designed to be used at home, on the go and even on a plane, therefore you'll always have all the oxygen you need, no matter where you are.
Concentrators also have the option of pulse-dose or continuous administration. Pulse-dose is a newer oxygen therapy technology that delivers oxygen through your cannula only when you breathe in. Continuous flow oxygen is constantly flowing through the tubes.
You should talk to your doctor about which dosing method is right for you. Pulse-dose technology can be delivered in a smaller size and will allow for longer battery life. Alternatively, most patients who require oxygen for sleep, use a continuous flow dosage due to shallow night breathing. Sometimes it's necessary to use continuous flow oxygen while you sleep and pulse-dose oxygen during the daytime.
Reference: http://www.oxygenconcentratorstore.com
Do Oxygen Facials Work?
Oxygen facial therapy has taken the beauty world by storm, with celebrities singing its praises and spas offering the treatment worldwide. But is this anti-aging wonder just another passing fad, or does it have scientific merit? Let's dive deep into the world of oxygen facials and uncover the facts behind this popular skincare treatment.
What is Oxygen Facial Therapy? Oxygen facial therapy is an innovative skincare treatment that involves applying pure oxygen to the skin, along with a cocktail of anti-aging ingredients.
The goal? To rejuvenate your complexion and achieve a more youthful, radiant look.
Key Benefits of Oxygen Facials:
- Firmer, more supple skin
- Reduced appearance of fine lines and wrinkles
- Less noticeable expression lines
- Improved blood circulation
- Enhanced complexion and skin tone
The Science Behind Oxygen Facial Therapy
Why Oxygen? Our bodies thrive on oxygen, and our skin is no exception. As we age, blood circulation decreases, leading to reduced oxygen delivery to skin cells. The theory behind oxygen facials is that by applying oxygen directly to the skin, we can:
- Boost cell oxygenation
- Maintain youthful-looking skin
- Enhance absorption of anti-aging ingredients
Oxygen facials often incorporate serums packed with:
- Vitamins
- Antioxidants
- Minerals
- Moisturisers
The high-pressure oxygen application is believed to help these beneficial ingredients penetrate deeper into the skin, potentially increasing their effectiveness.
Acne-Fighting Properties: Oxygen's bacteria-killing properties make it a potential ally in the fight against acne and other skin disorders, promoting a clearer complexion.
The Oxygen Facial Procedure
- Microdermabrasion: Removes dead skin cells and cleanses pores
- Oxygen Application: Uses an airbrush-like device to blast pure oxygen and anti-aging ingredients into the skin
- High-Pressure Delivery: Allows for deeper penetration of ingredients
Treatment Duration: 30-60 minutes
Immediate Results:
- Smoother, more hydrated skin
- Plumper appearance
- Reduced fine lines and wrinkles
- Improved skin colour and radiance
- Clearer complexion
Longevity of Results:
- Initial results last about 7 days
- Multiple treatments (6 sessions, once a week) can extend results to 1-3 months
Do Oxygen Facials Really Work?
While many swear by oxygen facials, it's important to note that scientific evidence supporting their effectiveness is limited. Critics raise several concerns:
- Inflammation: The plumping effect may be due to localized inflammation from high-pressure application.
- Free Radical Production: Increased oxygen levels might lead to free radical formation, potentially contributing to premature aging.
- Natural Alternatives: Aerobic exercise can naturally boost skin oxygenation through improved blood circulation.
FAQs About Oxygen Facial Therapy:
- Is oxygen facial therapy painful?
No, in fact, it's known for being a gentle and relaxing treatment. Most people describe the sensation as a cool, refreshing mist being applied to their face. - How often should I get an oxygen facial?
For optimal results, most skincare professionals recommend getting an oxygen facial once a week for six weeks as an initial treatment course. It's best to consult with a skincare specialist to determine the ideal schedule for your skin. - Can oxygen facials help with acne?
Yes, oxygen facials may help with acne. The high concentration of oxygen used in the treatment has antibacterial properties, which can help kill acne-causing bacteria. Additionally, the improved circulation and hydration can promote healing and reduce inflammation associated with acne. - Are there any side effects of oxygen facial therapy?
Oxygen facial therapy is generally considered safe with minimal side effects. Some people may experience temporary redness or slight swelling immediately after the treatment, but these effects usually subside quickly. It's always recommended to do a patch test or consult with a dermatologist before trying any new skincare treatment, especially if you have sensitive skin or any existing skin conditions. - How does oxygen facial therapy compare to other anti-aging treatments?
Compared to other anti-aging treatments, oxygen facial therapy is non-invasive and has no downtime, making it an attractive option for many. Oxygen facials are often seen as a good maintenance treatment or a gentler option for those new to anti-aging skincare.
Oxygen facial therapy continues to be a popular anti-aging treatment, despite the lack of conclusive scientific evidence. While many users report positive results, it's important to approach this treatment with realistic expectations and a balanced perspective. As always, a healthy lifestyle, proper skincare routine, and sun protection remain the cornerstones of maintaining skin health and longevity.
Oxygen can aid in Wound Healing
Oxygen is fast being recognised as one of the most powerful agents available to medicine. The therapeutic use of oxygen under pressure has been used to assist wound healing for almost 40 years.
It was first used to re-compress divers in the 1930s, and was developed to complement the effects of radiation in cancer treatment in the 1950s. Within a few years it was being used to support patients undergoing cardiac surgery, and to treat gas gangrene and carbon monoxide poisoning. Pressurized oxygen was first used to assist wound healing when it was noted in 1965 that burns of the victims of a coal mine explosion, treated with it for their CO poisoning, healed faster. In spite of this long history of therapeutic use, the mechanisms of pressurized oxygen are still being discovered and the medical use of oxygen under pressure is still an evolving speciality.
In wound healing, hypoxia can be defined as an insufficient supply of oxygen to allow the healing process to proceed at a normal rate and it is possible to have hypoxia in one area of a wound and not in an adjacent area.
Not all effects of hypoxia are bad and in fact all wounds initially have areas of hypoxic tissue. It actually causes several wound healing processes to occur but when hypoxia is severe, prolonged or widespread it can cause tissue cells to die and the wound can worsen and have effects on other parts of the body.
The capillaries can become leaky and oedema accumulates and blood circulation can become compromised. Surgery or medicine can re-establish circulation which sends blood to the ischaemic area, providing new oxygen substrate for the formation of more free radicals, with the result that the injury temporarily worsens. In massive injury the release of inflammatory cytokines and free radicals are high enough that it can lead to multiple organ failure. Therefore a catastrophic chain of events can be initiated by oxygen deprivation.
When used in wound healing pressurized oxygen is administered as a short pulse of oxygen - 90 minutes in a 24-hour day. Although the elevated amount of oxygen is only for a short time, the numerous other effects of pressurized oxygen carried on affecting and treating the wound after the treatment has stopped.
At elevated pressures the harmful effects of gas bubbles in the tissue are minimised.
The vasoconstrictive effects can be used to good effect and causes a significant reduction of oedema, which has been shown to be beneficial in re-perfusion injury, crush injury, compartment syndrome, burns and wound healing.
High levels of oxygen can diffuse into the wound which may otherwise be restricted if administered via the blood due to oedema or if blood vessels to the area have been damaged.
It is also capable of increasing the number of cytokines and many growth factors important to wound healing.
Pressurized oxygen also aids in the prevention of infection by not only the killing of bacteria, by aiding in providing an oxygenated environment which would kill of anaerobic organisms and increases the production of neutrophils which aid in also destroying bacteria but by also aiding and increasing the effectiveness of administered antibiotics.
Therefore pressurized oxygen has the potential to be used more widely in the future to aid in the healing of severe wounds and burns, as it has been proven to have reduced morbidity and infection, increases the healing process and reduces the extent of tissue necrosis and prevents further systemic problems in the body normally associated with severe wounds.
References:
http://www.worldwidewounds.com/2001/april/Wright/HyperbaricOxygen.html
Could We Destroy Cancer With Oxygen?
There is increasing interest in the theory that Oxygen therapy could be used to destroy cancer cells. Dr. Mark Sircus has published a book titled 'Anti-Inflammatory Oxygen Therapy' that discusses the use of oxygen itself as the ultimate chemotherapy and that doctors can blast cancer cells to smithereens, while patients sit in the comfort of their own homes.
Cancer shares a common vulnerability with viruses, bacteria and fungi all of who hate and cannot function efficiently in high levels of oxygen. When we send in unending waves of oxygen into cancer cells it behaves as if to soften them up before going in for the kill. Research scientists from the Cancer Research UK–MRC Gray Institute for Radiation Oncology & Biology at the University of Oxford have discovered that 'oxygen makes cancer cells weak and less resistant to treatment'.
Previously scientists have tried to cut off the blood supply and therefore oxygen supply which was thought to be fuelling tumour growth, with the idea to starve, shrink and kill the tumour. However, numerous studies have shown that tumour hypoxia (where the tumour is exposed to low oxygen concentrations) is in fact linked with more aggressive tumour behaviour and a poorer prognosis. It’s as if the tumour responds to low oxygen levels by growing and metastasising in order to seek out a new oxygen source.
When we use high oxygen levels as a treatment it actually improves the blood vessels within the tumours, thereby increasing the concentration of oxygen present. Instead of boosting a tumour's growth potential, it has the opposite effect and weakens the cancer cells from the inside, making them much more sensitive to radiotherapy or any other type of therapy.
Increasing your oxygen levels could offer amazing metabolism & immune function improvement. Most diseases thrive in low oxygen environments and keeping the body highly oxygenated could reduce the risk of many diseases. Oxygen therapy is also wonderful because more oxygen results in more cellular energy, more healing energy and more energy to help us feel good and perform better in life. And importantly, when enough oxygen rushes into oxygen deficient cells, there is instant energy available for detoxification of cellular poisons that have been building up. Many studies are being carried out into the use of pressurized oxygen therapy and it's effectiveness both solo and in conjunction with other treatments with various types of cancer. But based on early findings and theories, the potential in the future to be able to not only fight cancer effectively but to be able to do it reasonably cheaply, non-invasively and from the comfort of your own home is astounding.
References: http://drsircus.com and www.cancerresearchuk.org