Your Relationship With Your Oxygen Therapy
An interesting and unique paper has been researched and published, 'Explaining Adherence to Supplemental Oxygen Therapy:The Patient's Perspective' by Mark A Earnest. It looks at a group of COPD sufferers and investigates their use of oxygen therapy and the factors behind their varying adherence to their treatment regime.
For many people the level of adherence changes with time and reflects their struggle to manage their health, symptoms, physical ability and social issues. However adherence to oxygen therapy tended to increase with time as the realisation becomes apparent that a little compromise to lifestyle is required in order to reap the full benefits of oxygen therapy.
The barriers include the physical difficulty of using the oxygen, self-consciousness and a sense of social stigma, lack of perceived benefit, and fear of side effects from treatment.
The benefits far outweigh these barriers as supplemental oxygen therapy reduces mortality, improves sleep quality and general comfort, increases exercise tolerance, reduces pulmonary hypertension, normalizes heart rhythm patterns and improves cognitive brain function such as memory, intelligence, motor skills and perceptual motor ability.
The pattern of oxygen use adopted by any individual reflects their personal experiences and values and their efforts to optimally manage their lives. Four main areas affect adherence: functional management, health management, social management, and symptom management.
Functional Management
This is juggling the difficulty caused by weight and bulk, the perception that it hinders performing certain tasks with the benefit of improved fitness, strength, stamina and increased ability to perform these tasks.
Health Management
Individuals voiced concerns that they feared nasal dryness, nosebleeds and light-headedness. That they thought they may become addicted to it or that their lungs would become weakened.
These fears diminished as a result of personal experience. A realisation that the health benefits outweighed these fears and experience via an increase in use during episodes or on advice from a doctor.
Social Management
Social concerns relating to oxygen use, including embarrassment, self-consciousness, fear of burdening or inconveniencing others, concerns about appearing weak or sick, and a sense of shame, both about prior smoking and accepting dependence on a substance such as oxygen.
These elements tended to evolve over time. Some were able to overcome their fears or sense of self-consciousness by simply returning to a normal routine with family and friends. The desire to preserve independence and retain a high physical function and socialising helped them to overcome anysense of isolation and embarrassment. One woman described how,she felt once she followed her oxygen therapy fully:
'It opened a whole new vista for me. All of a sudden I was getting more active. I was doing the grocery shopping, and the laundry, and driving, and just becoming self-sufficient, which was what I used to do. I started volunteering then (in the rehab program) as a way of thanking them, you know, for saving my life.' (Female, age 69)
Symptom Management
The realisation that in most cases oxygen therapy helped to alleviate symptoms which resulted in a greater adherence to the treatment.
Management Balancing
Every participant in the study described some sense of compromise in the decisions they made regarding their use of oxygen. For most, the compromises were viewed as minimal or had been minimized by time and experience. In the four areas most patients realise that any uncertainties, fears or slight inconveniences in their lives were all far-outweighed by the benefits from oxygen therapy and adapted their lifestyles over time and through experiences and research, which generally resulted in an increased adherence to the treatment.
References: http://erj.ersjournals.com and http://www.ncbi.nlm.nih.gov
Plants may no longer be the sole producer of Oxygen
Earth's atmosphere hasn't always contained the Oxygen (O2) which is now essential for life, it was once a mixture of carbon dioxide and other gases, more like the atmosphere of Mars or Venus.

The only previously proven way that oxygen could have arisen is that the rise of plants turned the carbon dioxide present in the atmosphere into oxygen through the reactions of photosynthesis, in a period called the Great Oxygenation Event. However a new study suggests there may be another way to make oxygen from carbon dioxide, using ultraviolet light and that this method may in fact be partly or wholly responsible for the presence of Oxygen in our atmosphere.
Previously it was thought that a carbon dioxide molecule would split into a CO and an O molecule no matter what wavelengths of light were involved, because that is the path of least resistance and requires the least amount of energy in order to occur. O2 had not previously detected via these methods and therefore presumed to not occur.
However "when you shine C02 with these high wavelengths of light, it can break apart along more than one channel," said Cheuk-Yiu Ng, a professor of physical chemistry at UC Davis and an author of the paper. "These channels are energy dependent but at the energy we investigated, 5% of these excited CO2 would go on to become C+O2." The energy required for these 5% is double that which is required to split the molecule into CO + O.
Cheuk-Yiu Ng and his colleagues built a unique instrument to split up carbon dioxide, using ultraviolet light in a vacuum. The device has two lasers — one to split the CO2, and one to detect the fragments produced.
Therefore as certain ultraviolet rays pass through out atmosphere it is possible that 5% of the carbon dioxide molecules that they come in contact with will split and form oxygen molecules.
Not only does this potentially alter how scientists explain how oxygen first came to be in our atmosphere and effect the timeline of Earth's evolution but the findings have implications for future science. There may be implications on the search for extraterrestrial life, suggesting that merely detecting oxygen in the atmosphere of another planet is not enough to identify the presence of life. The researchers also hinted that it may be possible to use this technique to make oxygen in space or on other planets to aid in space exploration and settlement. Also instead of scientists extracting Oxygen molecules from the atmosphere for medical purposes among many others, we may be able to mass-produce oxygen using carbon dioxide in the future more easily.
References: http://www.latimes.com/science and http://www.livescience.com
Interesting facts about oxygen
Oxygen surrounds us and is fundamental for life and yet we can take it for granted and not realise that it's a lot more than just a component of the air.
- Our atmosphere today contains around 21 percent oxygen. About 300 million years ago oxygen levels reached 35 percent and insects were able to grow super-large- think dragonflies with the wingspans of hawks.
- Oxygen does not actually burn as people think it does. However it does support the combustion of other substances and without a supply of oxygen, combustion ceases. If you think about it, if oxygen itself actually burnt, simply striking a match would be enough to burn all of the oxygen in our planet’s atmosphere.
- Almost two-thirds of the weight of living things comes from oxygen, mainly because living things contain a lot of water and 88.9 percent of water’s weight comes from oxygen.
- Oxygen (O2) is very unstable in our planet’s atmosphere as it is very reactive and must be constantly replenished by photosynthesis in green plants. Without plant life, our atmosphere would contain almost no oxygen. If we discover any other planets with atmospheres rich in oxygen, we will know that life is almost certainly present on these planets as significant quantities of oxygen will only exist on planets when it is released by living things.
- The Northern (and Southern) Lights: The green and dark-red colours in the aurora Borealis (and Australis) are caused by oxygen atoms. Highly energetic electrons from the solar wind split oxygen molecules high in earth’s atmosphere into excited, high energy atoms. These atoms lose energy by emitting photons, producing awe-inspiring light shows. These usually occur in the polar regions because solar electrons will accelerate along our planet’s magnetic field lines until they hit the atmosphere in the polar regions.
- A common urban myth is that hyperventilation is caused by breathing in too much oxygen. When we hyperventilate, we breathe too quickly, and this can lead to symptoms such as headache, light-headedness, dizziness, chest pains, tingling, slurred speech, fainting and spasms. Hyperventilation actually causes us to get rid of too much carbon dioxide from our bodies. The trouble with this is that we need carbon dioxide in our blood to stop it from becoming too alkaline. When we hyperventilate, we lose too much carbon dioxide, which disturbs the balance of substances in our blood, causing its pH to increase; this causes the blood vessels leading to our brains to get narrower, slowing the blood flow and decreasing the amount of oxygen reaching vital organs, leading to the symptoms of hyperventilation.
- As a gas, oxygen is clear. However as a liquid, it's pale blue. If you've ever wondered what swimming in a pool of liquid oxygen would be like, the answer is very, very cold,(according to Carl Zorn of the Thomas Jefferson National Accelerator Facility). Oxygen must get down to minus 297.3 F (minus 183.0 C) to liquefy, so frostbite would be a bit of a problem.
References: http://www.chemicool.com/elements/oxygen-facts.html and http://www.livescience.com/28738-oxygen.html
FAQ's on supplemental oxygen
Why did my doctor prescribe oxygen for me?
Every body needs oxygen to survive. Every tissue and cell in the body needs a constant supply of oxygen to work properly.
The lungs breathe in oxygen from the air, then passes the oxygen into the bloodstream through millions of tiny air sacs called alveoli. Haemoglobin in the red blood cells then picks up the oxygen and carries it off to the body's tissues and cells.
Lung disease can cause inflammation and scarring in the alveoli. This inflammation and scarring makes it difficult for oxygen to move into the bloodstream. Therefore, the amount of oxygen in the blood drops, and the body's tissues and cells don't receive enough oxygen to keep functioning properly. Not enough oxygen in the bloodstream is called hypoxaemia.
Many diseases affect lung capacity and breathing and if your disease has progressed to a point where breathing is becoming increasingly difficult and you're suffering from hypoxaemia then your doctor may decide to start you with a prescription for supplemental oxygen.
How did my doctor determine that I need supplemental oxygen?
This will be determined by measuring the levels of oxygen in your blood. The amount of oxygen in the bloodstream can be easily measured in two ways:
-
Oximetry — A small, clip-on device shines a light through your finger or earlobe and measures the amount of light absorbed by the haemoglobin in the red blood cells. By calculating the amount of light absorption, the device can measure the percent of haemoglobin that is carrying oxygen, this result is known as the oxygen saturation of the blood. Normally this is around 95 to 100 percent.
-
Arterial blood gas study — Blood is drawn from an artery, usually in the wrist, using a needle and syringe. The blood is then sent through an analyser to measure the amount of oxygen gas dissolved in the blood. This result is called the arterial oxygen pressure, and is normally 80 to 100 mm Hg.
Cells and tissues cannot save up a store of oxygen, they need a constant steady supply. When the oxygen saturation falls below 89 percent, or the arterial oxygen pressure falls below 60 mmHg, whether during rest, activity or sleep, then supplemental oxygen is needed.
Your doctor can determine your supplemental oxygen needs by testing you while you are at rest and while walking, and can also order an overnight oximetry study to test your oxygen saturation at night.
When and how often do I have to wear my oxygen?
Your doctor will write a prescription for when and how much you should wear your oxygen, based on the results of your tests. The prescription should specify the following:
-
The appropriate oxygen flow rate or setting, expressed as litre flow of oxygen per minute that will keep your saturations at or above 90 percent
-
When you should wear your oxygen (during activity, overnight or continuously)
-
The type of equipment that you can use that will meet your lifestyle needs.
Why would I need to wear oxygen while sleeping?
Oxygen levels in the blood are naturally lower during sleep, due to a slightly reduced breathing rate and a reduced requirement by your body for oxygen. Also, some alveoli drop out of use during sleep. You naturally have a lower rate, however if your levels are already low as a result of your condition then they may faller dangerously lower during sleep.
If your waking oxygen saturation is greater than about 94 percent on room air, it is unlikely that your saturation during sleep will fall below 88 percent. However, your doctor can order an overnight pulse oximetry test if there is a question about your oxygen levels while you are sleeping.
How do I know that I'm using the right amount of supplemental oxygen?
To determine this your oxygen saturation must be measured while you are using your oxygen. Your doctor or a respiratory therapist from the oxygen supplier should test your oxygen saturation on oxygen while you are at rest, while walking and, if indicated, while you are asleep. As long as your oxygen saturation is in the 90s, you are getting the right amount.
Should I buy my own finger oximeter to test my oxygen saturations?
Some people feel more comfortable testing their own oxygen saturation throughout the day or during various activities, to make sure they are at least 90 percent saturated.
Finger oximeters are available on the Internet, through medical supply companies and even in sporting goods stores. They can be expensive however and have not been adequately tested for accuracy. You can speak with your doctor who can determine if a finger oximeter is necessary.
How will using supplemental oxygen benefit me?
A lack of oxygen to the body can result in damage to your organs, especially the brain, heart and kidneys. Wearing supplemental oxygen keeps these organs healthy. There is evidence that, for people who are hypoxaemic, supplemental oxygen improves quality of life and survival time.
Supplemental oxygen can also help relieve any symptoms from your disease. It can help relieve you from shortness of breath, fatigue, dizziness and depression. You may also be more alert, sleep better and be in a generally better mood. You may be able to do more activities such as travelling and generally feeling more mobile and able to get around and take part in hobbies.
Does my need for oxygen mean that I don't have long to live?
People live for years using supplemental oxygen but it will depend upon the progression of your disease and other complicating factors.
How long will I need to use supplemental oxygen?
That depends on the reason oxygen was prescribed. If your lung or heart condition improves, and your blood oxygen levels return to normal ranges without supplemental oxygen, then you don't need it anymore.
Can I become addicted to oxygen?
There is no such thing as becoming "dependent on" or "addicted to" supplemental oxygen, everybody needs a constant supply of oxygen to live. Your haemoglobin or cells wont adapt or structurally change in response to a constant higher supply of oxygen. They just use whatever oxygen is available to them.
Does supplemental oxygen cause side effects?
It is important to wear your oxygen as your doctor ordered it. If you start to experience headaches, confusion or increased sleepiness after you start using supplemental oxygen, you might be getting too much and need it to be altered.
Oxygen settings of 4 litres per minute or above can cause dryness and bleeding of the lining of the nose. A humidifier attached to your oxygen equipment or certain ointments can help prevent or treat the dryness.
Ref: http://www.ucsfhealth.org
An inadequate supply of oxygen contributed to cause of death cont...
Since the patients with even a single episode requiring intubation for severe asthma are at very high risk of recurring life threatening attacks and death, and since most asthma deaths take place at home, it is recommended that patients suffering with severe asthma provide themselves with supplemental oxygen at home for emergency use for possible attacks.
Around 1,600 adults and 20 children in the UK die every year from acute asthma. The key to their survival can be as simple as receiving a quick supply of pure oxygen.
However asthma sufferers are frequently told by their doctors and other healthcare workers that they do not fit the criteria for a home supply and many local GP surgeries do not hold emergency oxygen cylinders.
Research published in the British Medical Journal states that:
'an inadequate supply of oxygen was an important cause of death in those who died following a severe attack.'
The research suggests patients with severe asthma could be provided with oxygen cylinders for emergency use at home and says:
'The important point is that asthmatic patients are still dying during acute attacks - and the use of oxygen... in primary care is rational and could save lives.'
The research is supported by British Thoracic Society's guidelines which advise oxygen as a first line treatment for all patients with acute severe asthma. Asthma sufferers feel safer knowing that if oxygen is close to hand they will not only have treatment to save their life but it also reduces the severity of the attack; as stress and anxiety levels are reduced and quick and prompt treatment can halt the attack in its step.
An asthma attack may begin suddenly with wheezing, coughing, and shortness of breath. At other times, an asthma attack may come on slowly with gradually worsening symptoms. In either case, people with asthma usually first notice shortness of breath, coughing, or chest tightness. The attack may be over in minutes, or it may last for hours or days. Itching on the chest or neck may be an early symptom, especially in children. A dry cough at night or while exercising may be the only symptom.
During an asthma attack, shortness of breath may become severe, creating a feeling of severe anxiety. The person instinctively sits upright and leans forward, using the neck and chest muscles to help in breathing, but still struggles for air. Sweating is a common reaction to the effort and anxiety. The pulse usually quickens, and the person may feel a pounding in the chest.
In a very severe asthma attack, a person is able to say only a few words without stopping to take a breath. Wheezing may diminish, however, because hardly any air is moving in and out of the lungs. Confusion, lethargy, and a blue skin color are signs that the person's oxygen supply is severely limited, and emergency treatment is needed. Usually, a person recovers completely with appropriate treatment, even from a severe asthma attack. Rarely, some people develop attacks so quickly that they may lose consciousness before they can give themselves effective therapy. Such people should wear a medical alert bracelet and carry a cellular phone to call for emergency medical assistance. Research suggests a strong link between stress and asthmatic symptoms and experts suggest better treatment, including confident, self management of the condition, could improve the quality of life for asthmatics. The close links between stress and asthma are clear given the potential consequences of untreated attacks.
An asthma attack can be frightening, both to the person experiencing it and to others around. Even when relatively mild, the symptoms provoke anxiety and alarm. A severe asthma attack is a life-threatening emergency that requires immediate, skilled, professional care. If not treated adequately and quickly, a severe asthma attack can cause death.
People who have a mild asthma attack are usually able to treat it without assistance from a health care practitioner. Typically, they use an inhaler to deliver a dose of a short-acting beta-adrenergic drug such as albuterol , move into fresh air (away from cigarette smoke or other irritants), and sit down and rest.
People who have severe symptoms should typically go to an emergency department. For severe attacks, doctors give frequent (or sometimes continuous) treatment using inhaled beta-adrenergic drugs and sometimes anticholinergic drugs. Supplemental oxygen is also given immediately so as to increase the percentage level of oxygen being breathed in to help raise oxygen levels in the blood.
Since the patients with even a single episode requiring intubation for severe asthma are at very high risk of recurring life threatening attacks and death, and since most asthma deaths take place at home, it is recommended that patients suffering with severe asthma provide themselves with supplemental oxygen at home for emergency use for possible attacks.
An inadequate supply of oxygen contributed to cause of death
During an asthma attack, the smooth muscles of the bronchi contract, causing them to narrow, and the tissues lining the airways swell due to inflammation and mucus secretion into the airways. The top layer of the airway lining can become damaged and shed cells, further narrowing the diameter of the airway. A narrower airway requires the person to exert more effort to move the same amount of air in and out of the lungs. In asthma, the narrowing is reversible, meaning that with appropriate treatment or on their own, the muscular contractions of the airways stop, and the inflammation resolves so that the airways widen again, and the airflow into and out of the lungs returns to normal.

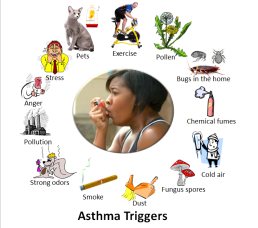
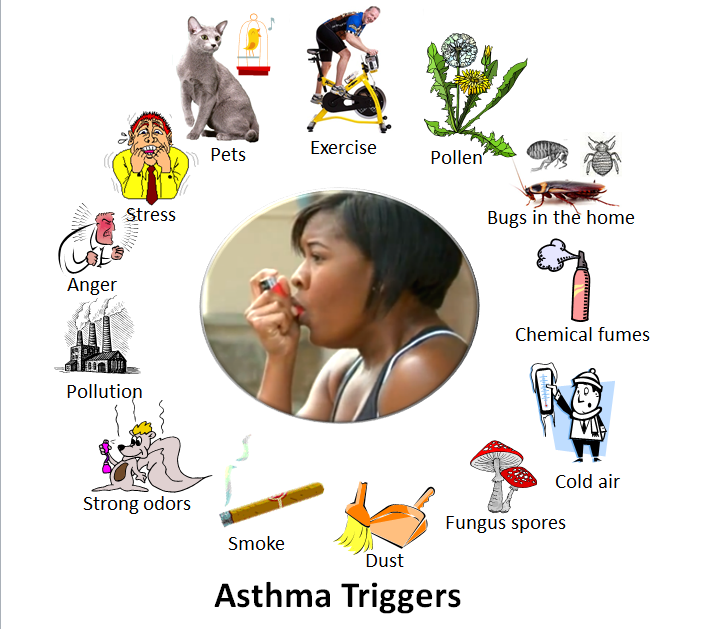
The airways narrow in response to stimuli that usually do not affect the airways in normal lungs (triggers). Such triggers include:
Allergens
Infections
Irritants
Exercise, stress, and anxiety
Aspirin
Many inhaled allergens can trigger an asthma attack, including pollens, particles from dust mites, body secretions from cockroaches, particles from feathers, and animal dander. These allergens combine with immunoglobulin E (IgE, a type of antibody) on the surface of mast cells to trigger the release of asthma-causing chemicals from these cells. (This type of asthma is called allergic asthma.) Although food allergies induce asthma only rarely, certain foods (such as shellfish and peanuts) can induce severe attacks in people who are sensitive to these foods.
Infectious triggers are usually viral respiratory infections, such as colds, bronchitis, and sometimes pneumonia.
Irritants that can provoke an asthma attack include smoke from tobacco, marijuana products, or cocaine, fumes (such as from perfumes, cleaning products, air pollution), cold air, and stomach acid in the airways caused by gastroesophageal reflux disease (GERD).
Additionally, people who have asthma can develop bronchoconstriction when exercising. Stress and anxiety can trigger mast cells to release histamine and leukotrienes and stimulate the vagus nerve (which connects to the airway smooth muscle), which then contracts and narrows the bronchi.
Asthma attacks can vary in frequency and severity. Some people are symptom-free most of the time, with only an occasional, brief, mild episode. Other people cough and wheeze most of the time and have more frequent and severe attacks.
An asthma attack may begin suddenly with wheezing, coughing, and shortness of breath. At other times, an asthma attack may come on slowly with gradually worsening symptoms. In either case, people with asthma usually first notice shortness of breath, coughing, or chest tightness. The attack may be over in minutes, or it may last for hours or days. Itching on the chest or neck may be an early symptom, especially in children. A dry cough at night or while exercising may be the only symptom.
During an asthma attack, shortness of breath may become severe, creating a feeling of severe anxiety. The person instinctively sits upright and leans forward, using the neck and chest muscles to help in breathing, but still struggles for air. Sweating is a common reaction to the effort and anxiety. The pulse usually quickens, and the person may feel a pounding in the chest.
In a very severe asthma attack, a person is able to say only a few words without stopping to take a breath. Wheezing may diminish, however, because hardly any air is moving in and out of the lungs. Confusion, lethargy, and a blue skin color are signs that the person's oxygen supply is severely limited, and emergency treatment is needed. Usually, a person recovers completely with appropriate treatment, even from a severe asthma attack. Rarely, some people develop attacks so quickly that they may lose consciousness before they can give themselves effective therapy. Such people should wear a medical alert bracelet and carry a cellular phone to call for emergency medical assistance. Research suggests a strong link between stress and asthmatic symptoms and experts suggest better treatment, including confident, self management of the condition, could improve the quality of life for asthmatics. The close links between stress and asthma are clear given the potential consequences of untreated attacks.
An asthma attack can be frightening, both to the person experiencing it and to others around. Even when relatively mild, the symptoms provoke anxiety and alarm. A severe asthma attack is a life-threatening emergency that requires immediate, skilled, professional care. If not treated adequately and quickly, a severe asthma attack can cause death.
People who have a mild asthma attack are usually able to treat it without assistance from a health care practitioner. Typically, they use an inhaler to deliver a dose of a short-acting beta-adrenergic drug such as albuterol , move into fresh air (away from cigarette smoke or other irritants), and sit down and rest.
People who have severe symptoms should typically go to an emergency department. For severe attacks, doctors give frequent (or sometimes continuous) treatment using inhaled beta-adrenergic drugs and sometimes anticholinergic drugs. Supplemental oxygen is also given immediately so as to increase the percentage level of oxygen being breathed in to help raise oxygen levels in the blood.
Part two to be continued....
Simply snoring and oxygen
Snoring can be a sign of sleep apnoea or other breathing conditions.
Types of Sleep Apnoea
1. Obstructive Sleep Apnoea: most prevalent, brought on by relaxation of the throat tissue
2. Less frequent, central nervous system involvement in central sleep apnoea
3. Complex sleep apnoea, which combines central and obstructive sleep apnoea
Sleep apnoea symptoms
- Experiencing drowsiness in the daytime
- Headaches when you first wake up
- Loud snoring followed by pauses and gasping for air
- memory loss or difficulty
- Irritable mood swings
- Need to go to the toile often at night
- Sore or dry throat in the morning
Left untreated there are potential risks to health such as:
- Gaining body weight
- Developing diabetes
- High blood pressure
- Potential strokes
Medical Sleep Apnoea Treatments
- Devices that provide continuous positive airway pressure (CPAP)
- Devices for oral hygiene
- Surgery (for more serious situations)
- Additional oxygen treatment
For individualised support, don't let these treatments stop you from travelling. You can take a look more at where and how it works over at OxygenWorldwide's website.
Fit to fly?
Billions of us travel by air each year however we are all individuals with varying needs, including a range of medical conditions and all airlines have different policies regarding this. For example some airlines will require a medical certificate to prove that you fit to fly.

The airline needs to ensure that air travel will not worsen or agitate a pre-existing condition and also that the patient’s ailment will not affect the comfort or safety of other passengers on the flight. Regardless of a doctor’s medical certificate the final decision remains with the airline and the captain of the flight and they may still refuse carriage.
A main considering factor involved in this decision making process is the affect of altitude, humidity and oxygen saturation levels during flight. Modern aircraft have a cabin altitude pressure equivalent of between 5,000 and 8,000 feet above sea level. (source: cyprusairways.com) This means that your blood will not be as saturated with oxygen and can affect breathing, cardiac activity, circulation and brain activity. Sometimes during flight, although not normally for long periods of time, a person’s oxygen saturation level can fall to 90%. A healthy individual can tolerate this temporary change with no problems however a patient with cardiac, anaemia or respiratory problems may find themselves in serious difficulties.
Aircraft cabins have low humidity levels that dry out the air; this can cause dryness of the skin or other mucous membranes within the body such as the throat and lungs and affect respiration.
Reduced cabin pressure can also cause gas volume expansion. Any gas that may have inadvertently been introduced to the body during surgery could then expand and cause pain or even perforation through the membrane.
A main deciding factor in whether or not a person may be considered ‘fit to fly’ is their oxygen saturation level. If a person’s saturation level is equal to, or more than 95%, they do not need oxygen for flying. If an asthma sufferer has a stable status then they should be able to fly as long as they keep their medication to hand. Anyone with an active exacerbation of respiratory disease should wait until their condition has improved before considering to fly. Consultation with a doctor or respiratory specialist will aid in ascertaining whether it is wise to fly or whether additional aids or medication would be wise to use during the flight. This may also help to persuade the airline that you are fit to fly.
As passengers sometimes cannot take their own oxygen equipment on board due to regulatory requirements although this is changing and more and more POC's (portable oxygen concentrators) are allowed on board of the aircraft.
If a passenger has used oxygen provided by the airline company he or she will have to pre-arrange oxygen at the end of the flight. OxygenWorldwide does provide an Airport Service where they have somone waiting at the door of the aircraft to hand over a portable oxygen device so one can travel onwards to their hotel or other holiday destination.
Please check with OxygenWoldwide for availability on your destination
Five reasons why travelling is easy with oxygen
1. Portable oxygen concentrators...




2. Oxygenworldwide has a huge network on a worldwide scale
3. OxygenWorldwide has a team of experts on hand prior to travel and during your holiday (SOS)
4. There are a wide selection of equipment types suitable for most oxygen patients
5. OxygenWorldwide have a multilingual team of staff
How oxygen can aid in severe altitude sickness

An Increasing number of people are now travelling to greater heights as it is becoming more readily accessible and cheaper to do so. However there can be adverse medical implications from doing so. Altitude sickness can affect people that ascend to more than 2500 metres of altitude, whether by climbing or being transported to these heights. It can also affect a person if they ascend too quickly for the body to adapt. It can present with mild symptoms that can subside when the individual has rested or returned to a lower altitude. However more extreme symptoms can be life-threatening if not counter-acted or treated.
Altitude sickness occurs because as you ascend to higher altitudes the air pressure reduces. The air still contains the same proportion of oxygen but as the air is thinner at higher altitudes there are fewer oxygen molecules available in each breath. This means that you have to breathe deeper and faster to obtain the same amount of oxygen that your body requires. If you ascend at a slow rate your body has a chance to acclimatise and adapt to the changing conditions. Your breathing rate will slow down as your body makes more red blood cells to carry more oxygen in your blood.
The most important initial treatment for someone displaying signs of altitude sickness is to stop the ascent and rest to allow the body to acclimatise. If symptoms persist then drop to a lower altitude. Normal symptoms illustrated by the body whilst it is acclimatising can be an increased breathing rate, deeper breathing, shortness of breath on exercise, changes to breathing patterns during sleep, disturbed sleep or passing more urine than normal.
If the affects of altitude are more severe than this then the body can display symptoms of the following three problems; acute mountain sickness, high-altitude cerebral oedema or high-altitude pulmonary oedema.
The exact cause of acute mountain sickness (AMS) is not known but it is thought to be a response of the brain to lower oxygen levels in the blood at higher altitudes which produces some swelling of the brain.
High-altitude cerebral oedema (HACE) usually develops in someone who already has acute mountain sickness (AMS). The swelling of the brain that has led to AMS gets worse and starts to interfere with the function of the brain. So, HACE is really a severe form of AMS.
High-altitude pulmonary oedema (HAPE) is a build-up of fluid within the lungs. The exact reasons why HAPE can develop are unknown. It is thought that the high altitude causes an increase in pressure in the blood vessels around the lungs which leads to smaller blood vessels becoming 'leaky', allowing fluid to escape from the blood vessels into the lungs.
The most important treatment if you start to develop symptoms of mild AMS is to stop your ascent and to rest at the same altitude. For most people, symptoms will improve within 24-48 hours with no specific treatment. Adapting to conditions (acclimatisation) usually occurs after 1 to 3 days at a given altitude. Simple painkillers and anti-sickness medication can help headache and sickness. You should also make sure that you drink plenty of fluids.
However, if your symptoms are severe, they do not improve after 24 hours, or they are getting worse, you need to descend to a lower altitude. You also need to descend urgently if you develop any symptoms or signs of HACE or HAPE.
Treatment of HACE and HAPE is similar and most importantly it is to move down to a lower altitude immediately. If this does not happen, or is delayed, death can occur. Treatment with oxygen and medicine can help to relieve symptoms and can mean that getting someone down to a lower altitude becomes easier. However, these treatments do not remove the need for descent. The descent should be at least to the last altitude at which the person woke up feeling well. A device has been developed called a portable hyperbaric chamber. It is, essentially, an airtight bag that is pressurised by a pump. The person with HACE is placed inside it and it can provide the same effect as a descent. They will be breathing air equivalent to that at much lower altitude. This can be life-saving when descent is not possible and oxygen is unavailable.
You can also use oxygen (small cylinder) to avoid these problems. OxygenWorldwide has on certain occasions arranged medical oxygen for mountain climbing. (For availability on your destination check with info@oxygenworldwide.com.