Spring is Finally Here-Not Good News for Some Oxygen Users

After the dreary winter months most of us are happy to see the early signs of spring; warmer weather, gentle breezes and flowers blooming however for oxygen, asthma and sleep therapy users these signs indicate the start of allergy season and suffering.
Allergies can be debilitating and can force sufferers to hide indoors to avoid flare-ups, can reduce the benefits and effectiveness of treatment and lower their quality of life.
Allergies affect your respiratory system through congestion and narrowing of airways and when you are already suffering from respiratory problems and are already requiring oxygen therapy, this additional problem can dramatically affect and worsen your condition.
With a bit of planning and awareness, you can minimize symptoms and live life to the fullest all year round.
KNOW YOUR PERSONAL ALLERGY SEASON
The term "allergy season" refers to certain months, in the spring and autumn when hay fever and airborne pollens are most prevalent out of doors, but your own "allergy season" will depend on where you live and what you're allergic to as different plants release pollens at different times of year and indoor allergies can occur all year round.
KNOW WHAT CAUSES YOUR ALLERGIES
In order to predict when you'll get allergies you need to know what is causing them. Allergies can be caused by a variety of indoor and outdoor pollutants.
KNOW THE SYMPTOMS
By recognizing the symptoms of allergies you can take action quickly when they hit. Stuffy or runny nose, ear congestion, sneezing, itchy or watery eyes, fatigue, excess mucus, sore throats, wheezing or coughing, and shortness of breath. More serious reactions such as rashes and swelling can also occur.
CLEANING
Indoor allergens, like dust and pet dander hide in bookshelves, air conditioning vents, window ledges, behind couches and under chairs. A good spring clean at the beginning of EVERY season can be a great way to make your home feel "new again" and it's a great way to minimize indoor allergens. For added protection wear a dust mask when you clean to keep exposure to a minimum; and only use mild soaps and detergents as required.
TOO MUCH FRESH AIR CAN BE HARMFUL
Enjoying fresh air and the great outdoors is one of life's great pleasures; but sometimes we can have too much of a good thing. Check the pollen count in your area and if it is high where you live try to stay indoors during the morning, when pollen counts are usually the highest, and on windy days, when dust and pollen are blown about. Keeping windows closed at night, and using air conditioning instead, can also help keep pollens and moulds from drifting into your home; and air conditioning can also clean and dry the air.
KEEP YOURSELF EXTRA CLEAN
Shower and wash your hair daily; every night if possible, to help clean off any allergens that have gathered on your body during the day. Don't mow lawns or rake leaves as this can stir up pollens and dust; and instead of hanging clothing outside to dry, dry it inside to keep it away from airborne pollens and moulds.
TAKE CARE OF YOUR SLEEP, ASTHMA & OXYGEN EQUIPMENT
Dust, pollen, moulds and allergens don't react well inside your lungs and sinuses and they're no good for sleep, oxygen and asthma therapy equipment either:
Many oxygen concentrators have filters that need to be changed or replaced on a regular basis. Air inlet filters are often external to the machine and should be washed and thoroughly dried on a regular basis. Internal filters usually only need to be replaced every few years. In addition oxygen cannulas and tubing should be replaced regularly to ensure that moulds and bacteria don't build up.
USE AN APP ON YOUR PHONE
There are now free apps available to download onto your phone that can help you monitor allergic events, you can keep a diary and it can alert you to when the seasons are due to start. It also will keep track of lots of medical data so that you can then show to your doctor to discuss any possible requirements to alter medication or oxygen flow rates or equipment.
TAKE A VACATION
This may be the ultimate vacation excuse so why not take a vacation during the height of your allergy season. Go to the beach or any clean, pollen-free area and enjoy an allergen free vacation. The relief from the additional suffering and the fact that you're having a holiday will be blissful and beneficial to your health and well-being.
Remember that NHS oxygen providers don't supply oxygen to travel abroad, but its easy to organise any oxygen requirements you might have if you need to travel or fly abroad, just visit our website www.oxygenworldwide.co.uk.
References: http://www.directhomemedical.com and http://www.efanet.org
The 6 Other Major Symptoms of COPD
COPD includes two different lung diseases: emphysema and chronic bronchitis. People with these conditions have damage to the airways and the air sacs inside their lungs. This damage makes it harder for them to breathe and to get enough oxygen into their bodies with each breath. COPD produces many outward symptoms, which slowly get worse over time and all of which originate from the lung and airway damage. The main and most commonly known symptom is the difficulty to breathe and the requirement for Home Oxygen Therapy, where patients can use oxygen at home to help ease their symptoms.
1. Mucus-Producing Cough
The cough is the most obvious symptom of COPD. The damage to the lungs causes them to produce more thick mucus than normal which can block the airway and make it difficult to breathe. Coughing it up is the body's natural and most efficient way to clear it from the body. One way to ease a phlegmy cough is to drink extra fluids, which helps loosen up the mucus so the body can remove it more easily.
2. Wheezing
With COPD the air that you inhale with each breath has to travel down narrowed airways. The air struggles to get through and causes the walls of the airways to vibrate. This vibration combined with moving air produces a whistling sound which we call wheezing. Bronchodilators and steroid medicines can be given to widen the airways and relieve the wheezing and ease breathing.
3. Blue Lips and Nails
This condition can also result in your lips and nails turning a bluish colour. This illustrates the lack of oxygen being delivered to those parts of the body and an indication that there isn't enough oxygen in your blood generally. Normally, the blood is red but when it’s deprived of oxygen, blood turns blue which gives the lips and fingernails their blue hue. A bluish discolouration of the skin is also called cyanosis. It’s a very serious symptom as it indicates extremely low oxygen levels and if noticed an immediate call for emergency medical care should be made.
4. Lower Body Swelling
To compensatge for the damage to your lungs, your heart has to pump harder to get enough oxygen to your body. Over time the heart muscle can become damaged and enlarged from the extra work and lower body swelling is an indicator of this. The heart doesn’t beat as forcefully as it should and low blood pressure could lead to a blood clot if not treated.
5. Barrel Chest
Long term sufferers may develop a bulging in their chest which takes on a barrel-like appearance, called a barrel chest. This can form because your lungs are so filled with air that they eventually stretch out your ribcage. A barrel chest can worsen existing breathing problems from COPD, making it even harder for you to catch your breath.
6. Weight Loss
With your lungs not working as well your body has to exert more energy than normal to try to compensate and maintain minimal oxygen levels. This causes you to burn up to 10 times more calories than usual and can result in hunger and fatigue if the calorie intake is'nt increased. Shortness of breath and coughing can also make you less interested in eating and with this combination over time, you’ll start to lose weight. Any weight loss in COPD is a serious sign and when your body is too thin, it can’t protect you as well against infections.
References: http://www.healthline.com
Are There Side Effects To Oxygen Therapy?
Oxygen therapy is a crucial treatment for many individuals with respiratory conditions. While it's generally safe, it's important to understand the potential side effects and risks associated with this treatment.
The Nature of Oxygen Therapy Side Effects
- Oxygen is a natural substance our bodies use daily
- Side effects are primarily due to administration methods or oxygen volume
- Fewer side effects compared to many other medical treatments
Common Side Effects of Oxygen Therapy
1. Nasal Discomfort
- Dry or bloody nose
- Can often be resolved with nasal sprays or humidifiers
2. Skin Irritation
- Caused by nasal cannula or face mask
- Resolvable with alternative devices or over-the-counter gels
3. Fatigue and Headaches
- Morning headaches
- Tiredness
4. Transtracheal Oxygen Therapy Complications
- Mucus build-up
- Potential for infection
- Risk of windpipe injury
Managing Side Effects
- Communicate persistent issues to your doctor
- Adjustments to flow rate or usage time may help
- Consider using a humidifier with your oxygen equipment
- Explore alternative oxygen delivery devices for better comfort
Safety Considerations for Oxygen Use
- Follow provider's safety guidelines strictly
- Proper storage of oxygen equipment
- Awareness of oxygen's combustible nature
- Regular cleaning and maintenance of equipment
The Benefits Outweigh the Risks
- Improved quality of life
- Enhanced mobility
- Better social interaction
- Increased longevity
Consult Your Doctor If:
- Side effects persist or worsen
- You experience new or unexpected symptoms
- You have concerns about your oxygen therapy regimen
While oxygen therapy may come with some side effects, most users find them manageable and far outweighed by the benefits.
Breathing Extra Oxygen Can Help Fight Cancer
A study in mice has suggested that by doing something as simple as breathing in extra oxygen may provide our immune cells with an extra boost to fight cancer.

The immune system often can spot and destroy abnormal cells before they grow into cancer. Normally cancer tumour cells put up defences in order to block our immune system from attacking them. One way they do this is because tumours can grow so rapidly that they outpace their blood supply, creating a low-oxygen environment. By maintaining low oxygen levels inside the tumour, this can increase the production of a molecule that blocks the tumour fighters that our immune system produces, called T cells. Lots of research is under way to develop drugs that could block the production of this molecule adenosine, but researchers at North Eastern University wondered whether adding oxygen to tumours could strip away that defence. So they put mice with lung tumours into chambers that let them breathe oxygen doses mimicking supplemental oxygen therapy doses.
The results showed that tumours shrank more in the high-oxygen group, and even more so when researchers also injected the mice with doses of extra T cells. With the extra oxygen, "you remove the brake pedal" that cancer can put on tumour-fighting immune cells, said Michail Sitkovsky, director of the New England Inflammation and Tissue Protection Institute at North Eastern University, who led the work. The extra oxygen changed the tumour's environment so that immune cells could get inside and do their jobs.
The study has exciting potential but obviously it must be tested in people first. If it works then this supplemental oxygen approach could be utilised to work in conjunction with other cancer therapies to aid in the battle against cancer.
References: http://www.usnews.com and http://blackburnnews.com
How Do Different Devices Provide My Oxygen?
Oxygen therapy is administered in a variety of ways depending upon the circumstance, the patient's requirements and the devices used. It is required in order to provide additional oxygen to the patient and to increase the level of oxygen in the body needed by your body to function.
In most cases the oxygen first passes through a pressure regulator which controls the oxygen pressure as it passes from an oxygen cylinder to the device which is at a lower pressure. Once the oxygen is at this lower pressure, the flow of the oxygen can be controlled by a flow-meter and is measured in litres of oxygen per minute (lpm). The usual flow rate for most devices is between 0 and 15 lpm but can be as high as 25 lpm in some units. Many flow-meters are based on a 'Thorpe tube' design which can be set to 'flush' which is useful in an emergency situation.
In room air the content of oxygen is only 21%, which although is adequate for healthy individuals, needs to be increased to help those with certain diseases or medical conditions in order to increase the oxygen that manages to get through to their blood stream. Usually increasing the oxygen to 30-35% is enough to make a significant difference and this can be achieved using a nasal cannula, a thin tube with an individual tube for each nostril. This can provide the oxygen at a low flow rate (0.25 to 6 lpm) to achieve an oxygen level of 24-40%.
To achieve higher oxygen concentrations various face masks can be used including a simple face mask, which can deliver oxygen at 5-15 lpm to achieve 28-50% oxygen levels. The Venturi mask can provide oxygen up to 40% and a partial re-breathing mask, which includes a reservoir bag attached to it can provide oxygen at between 40% and 70% concentration.
For patients requiring 100% oxygen the most common device is the non-breather or reservoir mask. This is similar to the re-breathing mask but has a number of valves to stop air that has been exhaled from the lungs from returning to the bag. At a flow rate of 10 lpm up to 80% oxygen levels can be achieved.
For patients requiring the therapy on a constant long-term basis, the oxygen can be warmed and humidified before administration through the nasal cannula to prevent irritation and dryness.
If a patient cannot breathe independently then positive pressure may be needed to force air into the lungs, which is provided by complex artificial respirator machines such as ventilators or a continuous positive airway pressure machine.
References: http://www.news-medical.net and http://www.nhs.uk/conditions/home-oxygen
Travelling with Oxygen: How Does My Oxygen Concentrator Work?
Over the years, portable oxygen technology has developed and combine with travel really assists in maintaining those who require supplemental oxygen the ability to travel across the globe. This article explores these developments, the safety aspects and tips for oxygen assisted travel today.
Understanding Portable Oxygen Concentrators or (POCs)
Portable Oxygen Concentrators mean that you can have your oxygen therapy as you move. These compact devices:
1. Extract oxygen from ambient air
2. Deliver purified oxygen to the user
3. Operate on rechargeable batteries
4. Are approved for use on most airlines
How POCs Work
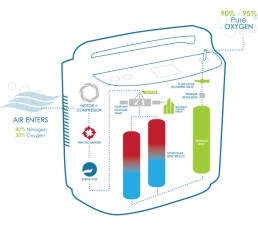
POCs utilise 'pressure swing adsorption' technology:
1. Compress ambient air
2. Remove nitrogen using zeolite minerals
3. Concentrate oxygen to 90-95% purity
4. Deliver oxygen via pulse or continuous flow
Latest POC Innovations
- Lighter weights (some under 5 lbs)
- Extended battery life (up to 8 hours)
- Smart device connectivity for monitoring
- Quiet operation for discreet use
Travel Planning with Oxygen
1. Consult Your Doctor
- Obtain travel clearance
- Discuss oxygen needs at different altitudes
2. Contact Airlines in Advance
- Confirm POC approval
- Arrange for in-flight power sources if needed
3. Pack Essential Supplies
- Extra batteries
- Power adapters for various outlets
- Nasal cannulas and tubing
4. Research Destination Healthcare
- Locate oxygen suppliers at your destination
- Know emergency medical facilities
5. Consider Travel Insurance
- Ensure coverage for oxygen-related needs
Safety Tips for Oxygen Travel
- Keep POC in carry-on luggage
- Bring prescription and doctor's statement
- Avoid smoking areas and open flames
- Stay hydrated, especially during air travel
Choosing the Right POC for Travel
Factors to consider:
- Flow rate requirements
- Battery life
- Weight and size
- Noise level
- FAA approval status
Overcoming Travel Challenges
- High-altitude destinations: Consult your doctor about adjusting oxygen flow
- Extended trips: Research oxygen refill options at your destination
- International travel: Check voltage compatibility and plug adapters
The Future of Oxygen Travel
Emerging technologies promise even more freedom:
- Wearable oxygen devices
- Improved battery technology
- Integration with smart health monitoring systems
With proper planning and the right equipment, oxygen therapy users can explore the world with confidence.
The Difference Between Pulse And Continuous Flow
At OxygenWorldwide, we understand that oxygen therapy shouldn't limit your wanderlust. Let's explore how portable oxygen concentrators (POCs) are revolutionizing travel for those who need supplemental oxygen.
The Evolution of Portable Oxygen
Since 2000, POCs have transformed from bulky machines to sleek, travel-friendly devices. They offer two main types of oxygen delivery:
1. Continuous Flow: Ideal for patients with high oxygen needs
2. Pulse Flow (On-Demand): Perfect for more active users
Continuous Flow POCs: Steady Support
• Provide uninterrupted oxygen supply
• Preferred by patients with severe respiratory issues
• Offer mobility, but may use oxygen faster
Pulse Flow POCs: Efficiency Meets Portability
• Deliver oxygen only when you inhale
• Conserve oxygen, extending usage time
• Lightweight (around 2kg) and highly portable
• Suitable for high-altitude travel
Dual-Flow POCs: The Best of Both Worlds
• Combine pulse and continuous flow options
• Cater to a wider range of oxygen needs
• Slightly heavier (5-10kg) but often come with wheels
Choosing Your Perfect Travel Companion
When selecting a POC for your adventures, consider:
1. Your prescribed oxygen flow rate
2. Battery life and charging options
3. Weight and portability
4. Altitude performance
5. Noise levels
Sleep Considerations
• Pulse-flow POCs may not be ideal for all sleep situations
• Some modern POCs adjust to slower nighttime breathing
• Continuous-flow mode is often preferred for CPAP users
OxygenWorldwide's Travel Tips
1. Consult your doctor about your travel plans
2. Familiarize yourself with your POC's features
3. Carry extra batteries and charging accessories
4. Know your oxygen needs at different altitudes
5. Check airline policies before booking
The Future of Oxygen Travel
At OxygenWorldwide, we're excited about emerging technologies that promise even greater freedom:
• Smarter, more responsive POCs
• Longer-lasting batteries
• Integration with health monitoring apps
Conclusion
Don't let oxygen needs ground your travel dreams. With the right POC and proper planning, the world is yours to explore. OxygenWorldwide is here to support your journey every step of the way.
Misdiagnosis of COPD is Common and Dangerous
There are many stories of patients being misdiagnosed and given treatment for asthma when in fact years later the patient is then diagnosed with COPD.
Pat Crowe was a healthy, active 39 year old but was told he had developed asthma and was given an inhaler. Over the next few years his health deteriorated, he grew dependent upon and overused his inhaler, suffered from side effects and eventually the inhaler wasn't enough. Being so breathless meant his confidence plummeted, making him almost housebound.
'I panicked about going outside and crossing busy roads because I was having trouble breathing and couldn't move quickly.'
During bad spells and prolonged attacks he was also prescribed strong steroid pills, which caused side-effects, including a swollen face and hunger.
'My wife became my carer, and my family were very scared watching me struggle to breathe,' he says. 'I didn't even want to get out of bed and go down stairs because I was worried about getting back up. My life changed completely.'
It was only then that Pat's consultant performed a spirometer test which confirmed that he didn't have asthma after all but suffered from COPD, which explained why he'd found the condition impossible to control.
COPD is incurable and affects 900,000 people in the UK, usually above the age of 35, and an estimated 30,000 people die from it each year. Experts believe there are also more than two million undiagnosed cases.
Specialist advice is crucial when it comes to achieving an accurate diagnosis says Dr Kurukulaaratchy: 'GPs need better awareness of these conditions. They both rank highly in hospital admissions, but if management is right early on, you can improve quality of life and possibly even life expectancy.'
Nick Hopkinson, honorary chest physician at the Royal Brompton Hospital, London, adds: 'Asthma patients usually have normal lung function, but when they experience asthma symptoms or an attack their airways go into spasm, becoming narrow and inflamed. Then, after taking medication - usually an inhaler - their lungs return to normal. However, COPD patients have relatively fixed lung disease, so even on a good day they still have symptoms. Most of the damage isn't reversible and progressively worsens.'
One major consequence of misdiagnosis is that patients could be given the wrong medication.
COPD patients usually start with bronchodilator inhalers to relieve narrowing of the airways and then go through a variety of drugs, starting with shorter-acting medications and moving to longer-acting ones, as the disease worsens, says Dr Kurukulaaratchy.
'Research has shown steroids can lead to an increased risk of pneumonia (inflammation of lung tissue) in COPD patients, so this is a risk if they are wrongly labelled as having asthma.'
If the condition doesn't improve, they can end up using a lot of steroids, which have side-effects such as weight gain, mood changes and osteoporosis.
'If patients are told they have COPD but it's asthma and they don't have inhaled steroids, they won't be able to control the disease - leaving them prone to worsening symptoms and even death from an asthma attack,' says Dr Hopkinson. 'We see 1,100 asthma deaths a year in the UK, often because they weren't on preventer treatments.'
Also oxygen therapy treatment is a major component of COPD treatment which is prescribed by your doctor, so if you are misdiagnosed then you may not be prescribed oxygen as early as you should have been which can affect your health and long-term diagnosis as COPD damage to the lungs is irreversible.
If you have any doubts about your diagnosis then speak to your doctor or get a second opinion, just to be sure as your health is the most important thing.
References: http://www.dailymail.co.uk
Lifestyle Tips To Manage Your COPD
Living with chronic obstructive pulmonary disease (COPD) doesn’t mean you have to stop living your life. Being on the correct medication and oxygen treatment regime is crucial but there are some tips on lifestyle changes that you can make to help you manage the disease.
Stop Smoking
Smoking is the number one cause of chronic bronchitis and emphysema. Together these diseases comprise COPD. If you haven’t already quit, it’s very important to take steps to stop smoking. Talk to your doctor about smoking cessation strategies.
If nicotine withdrawal is a concern, your doctor may be able to prescribe nicotine replacement therapy to help you slowly wean yourself off. Products include gum, inhalers, and patches.
People with COPD should avoid all inhaled irritants such as air pollution, dust, or smoke from wood-burning fireplaces.
Defend Against Infections
People with COPD are at risk for respiratory infections, which can trigger flare-ups. Infections that affect the airways can often be avoided with good hand-washing hygiene. Cold viruses, for instance, are often passed through touch. Simple soap and running water do a good job of removing potentially infectious germs.
It may also be helpful to avoid contact with people who show signs of cold or flu. Your doctor may also recommend an annual flu vaccine.
Focus on Good Nutrition
Eating right is an important way to keep your body and your immune system strong. It may be helpful to eat smaller meals, more often. Try to eat a diet rich in fruits, vegetables, fish, nuts, olive oil, and whole grains. Cut back on red meat, sugar, and processed foods. Following this dietary pattern has been shown to help reduce chronic inflammation, while supplying plenty of fibre, antioxidants, and other nutrients to help keep you healthy.
Your doctor may also recommend nutritional supplements to ensure you’re getting the essential nutrients you need.
Tend to Your Emotional Needs
People living with disabling diseases such as COPD occasionally succumb to anxiety, stress, or depression. Be sure to discuss any emotional issues with your doctor as they may be able to prescribe medications to help you cope or also recommend other approaches to help you cope. This might include meditation, special breathing techniques, or joining a support group. Be open with friends and family about your state of mind and your concerns and let them help in any way they can.
Stay Active and Physically Fit
Research shows that exercise training can improve exercise tolerance and improve quality of life among people with mild to moderate COPD. It can also help provide relief from shortness of breath and improve your mental well-being.
Asking for portable oxygen devices from your supplier can aid you in being more mobile and to have oxygen with you whilst you exercise or carry out more strenuous activities.
References: http://www.healthline.com
O-X-Y-G-E-N
O - Options - Ask your supplier for devices or gadgets to help suit you and your home.
X - eXpectations - Medical advancements and oxygen supply companies have come a long way but you should have high expectations for your health, talk to your doctor and make sure you use a reputable, caring oxygen supplier.
Y - Your lifestyle - This can still be maintained with a little oxygen help, especially with portable oxygen devices - keeping active is important!
G - Go on Holiday! - There's no reason why people using oxygen cannot go on holiday, from flights to cruises to mini-breaks abroad by car, just ask your oxygen supplier to help arrange and cater for your oxygen requirements!
E - Enjoy a Long Life! - With improved portable oxygen devices to help you keep mobile and improved medical treatments and drugs, life expectancy has greatly improved and patients live a long, near normal life nowadays.
N - Needs Change - Your disease may improve or worsen or your general fitness may alter and so will your oxygen requirements. Always attend your check-up appointments so that your doctor can alter your oxygen prescription accordingly.